|
|
 |
|
- Americans in 2001 were overweight or obese 66%; compared with 65% in 1999-2000.
- The number of obese Americans was also unchanged -- 31%.
The number of extremely obese Americans
was also unchanged -- 5%.
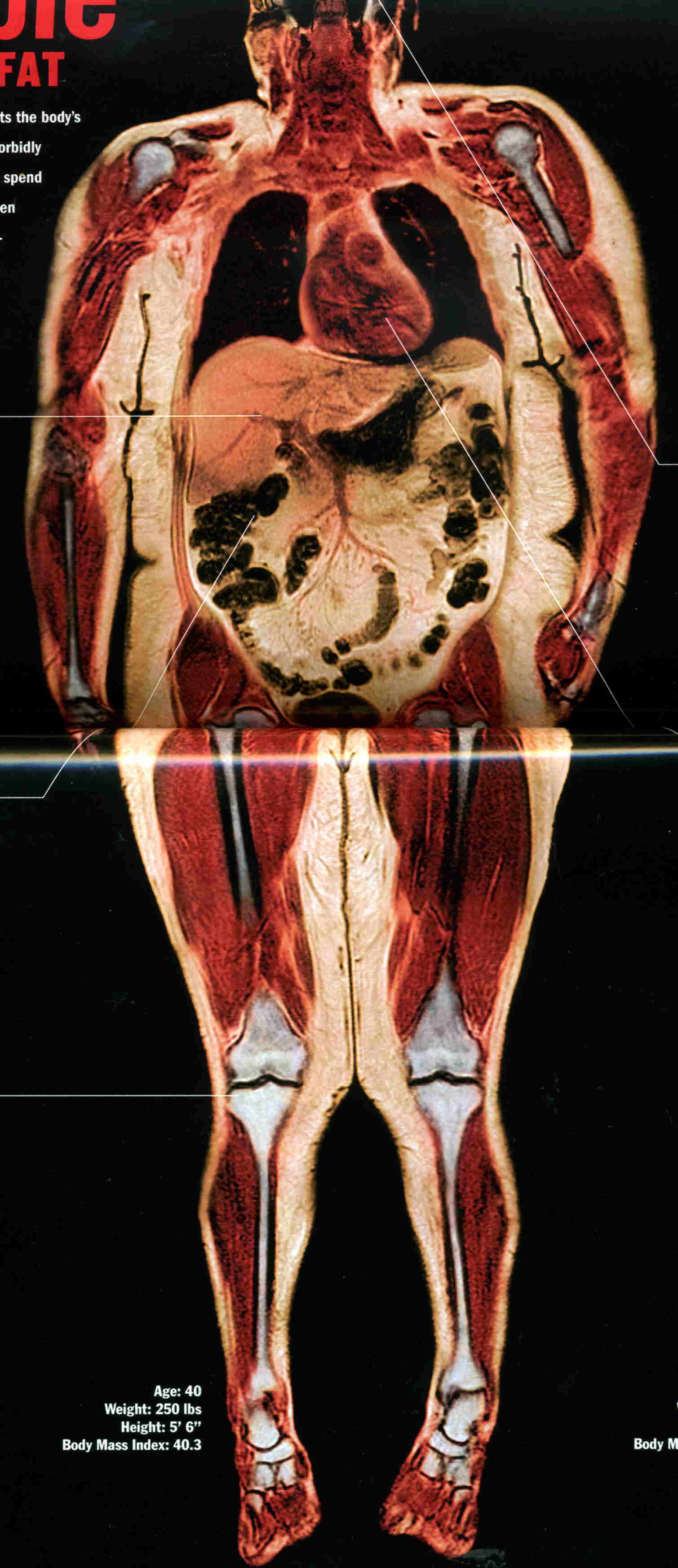
Obesity hurts: 1) quality
of life, 2) sexual performance), 3) shortens life on an average 5 years.
|
 |
|
|
| From Scientific American article |
The article goes on to point out that obesity is learnt (behavioral)
not genetic in nearly all instance. The article compares a genetically identical group for which there
were recent changes in financial and cultural circumstances. The Pima Indians who in Arizona have a high
prevalence of obesity while just across the boarder their relatives are typically lean. Undoubtedly there
are genetic factors, however, as with the Pima Indians, cultural pressures have been shown to control this disposition to
becoming grossly fat.**
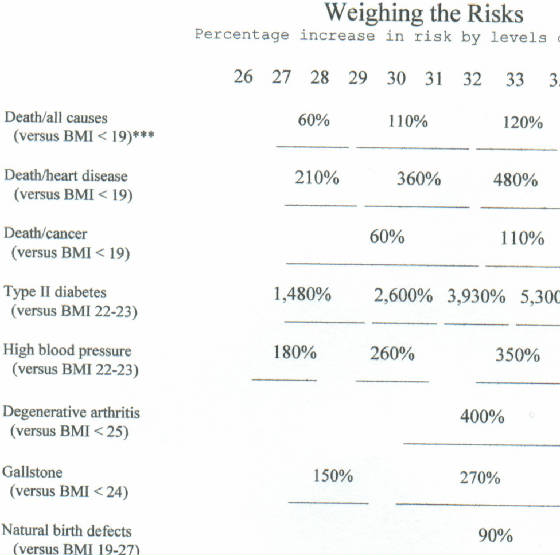
* BMI (Body
Mass Index) is computed by taking the weight in kilos and dividing by the height in meters squared (B/M2).
There are 2.2 lbs per kilo, and 39.37 inches per meter. For 6 feet and 160 lbs
the BMI is 22.0, for170 lbs, BMI 23.2, and for 250 BMI 34.3. For 5feet 6 inches 120 lbs, BMI 19.4, and
for 130 lbs the BMI is 21.0; for 180 lbs the BMI is 29.1. It should be noted that women, who because of
less muscles when lean weigh less than a man of the same height who is equally lean, that such woman on an average are longer
lived. Thus the higher BMI for the lean man than a lean woman is consistent with the longevity of woman.
** Though
not made in the article, I should point out that any trait which is disadvantages, either to survival or reproduction, will
become rare. This has been proven by numerous population studies. Obese people reproduce
less; therefore, any and all genetic causes would become rare. Thus like smoking obesitys primary causes must be social.
^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^
A recent study found a very strong connection between alzheimer's disease and obesity. For those over 50% above their
lean body mass the increase risk was over 150%, another found a over 60%.increased risk of dying from cancer for those with
a BMI over 40.
^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^
U.S. Is Still a Nation of Excess
Childhood Obesity, Adult Obesity Are Still Big Problems
June
15, 2004 -- A new study provides a snapshot of the nation's obesity problem -- and it's not a pretty picture. More than half
of adults are still overweight or obese, and one-third of children is at risk for overweight or is overweight.
From
1999 to 2002, the number of overweight Americans continued to increase, according to the nationwide survey from the CDC. It
is published in this week's Journal of the American Medical Association (JAMA).
"There
is no indication that ... obesity among adults and overweight among children is decreasing," writes researcher Allison A.
Hedley, PhD, with the CDC. "The high levels ... remain a major public health concern."
Between
1999-2000 and 2001-2002:
- Americans were still overweight or obese -- 66% -- compared
with 65% in 1999-2000.
- The number of obese Americans was also unchanged -- 31%.
- The number of extremely obese Americans was also unchanged
-- 5%.
From 1999 to 2002:
- More than 50% of adults were overweight or obese; this was
true in almost every age and racial/ethnic group.
- 28% of men over age 20 were obese across all racial and ethnic
groups.
- 33% of women over age 20 were obese -- but with significant
differences among racial and ethnic groups.
- 49% of all black women were obese, compared with 38% of Mexican-American
and 31% of white women.
- 14% of black women were extremely obese -- the highest number
of any ethnic/racial group, whether male or female.
Among children:
- 30% were overweight or at risk for being overweight in 1999-2000
versus 32% in 2001-2002.
- 15% were overweight in 1999-2000; 17% were in 2001-2002.
- Black and Mexican-American children were at a significantly
greater risk of becoming overweight, compared with white children.
There is no indication that obesity in adults and children is decreasing, Hedley concludes.
This articles ties the pieces together.
High levels of blood glucose has been know of decades to be associated with aging and coronary disease.
This article describe the varied effects of the failure to regulate the level of glucose due to insulin resistance.
Obesity is the most significant cause of insulin resistance.
THE
INSULIN CONNECTION
U.S. NEWS.COM
By Brenda Goodman Mon Aug 29, 5:33 PM ET
Diabetes drugs have made a big difference to George Marincin
and Kristin Chapman. For a few weeks last year, Marincin, 77, from Tacoma, Wash., took artificial insulin, the hormone that's
deficient in diabetics. And every day Chapman downs doses of Glucophage, a drug that helps the 38-year-old from Atlanta to
better control the hormone.
But neither Marincin nor Chapman has
diabetes.
What Marincin does have is Alzheimer's disease. He took insulin to test the idea that low levels
might be linked to memory problems. "I did wonder how insulin could help George because he's not diabetic," says his wife,
Mabel. "But it has. It's wonderful." Her husband has regained his sense of humor and can even complete simple tasks again
like making a cup of tea, she says. Last month his doctors reported in the Archives of Neurology that other patients
also seemed to benefit.
Chapman was just as surprised that adjusting insulin
levels could help her. She has polycystic ovary syndrome, which causes infertility and dramatically raises her risk for heart
disease. But her problem wasn't too little insulin but too much, which prevents ovulation. After seven years of struggling
to conceive, she started taking Glucophage and was pregnant in a month. "It's mind boggling, isn't it?" she says. Now the
happy mother of two kids, she'll stay on the drug for the rest of her life to keep her high insulin in check.
Insulin problems--too much or too little--go far, far
beyond diabetes. The condition is called insulin resistance and, in addition to the ailments dogging Chapman and Marincin,
doctors are now discovering it is linked to heart attacks, strokes, and several kinds of cancer and may affect 1 in 3 American
adults. These findings have alarmed many specialists. "Insulin resistance is very common, and it's associated with the biggest
killers," says endocrinologist Ronald Kahn, director of the Joslin Diabetes Center at Harvard University. "If we don't start
paying attention to this now, we're all going to be paying a huge price for this condition." Physician David Katz, director
of the Prevention Research Center at Yale Medical School, adds that "we're just beginning to understand that insulin throws
a lot of big switches in the body. Is insulin the master control of all disease? I don't know, but it's certainly a
candidate for that role."
Insulin's main job is to escort sugar out of the blood
and into muscle and fat cells. But sometimes those cells resist letting it in. So the pancreas, which makes insulin, tries
to crank out even more. If it can't, blood sugar climbs to dangerous levels and the result is Type II diabetes. More often,
however, the pancreas does make more insulin. The extra hormone may restore blood sugar to normal, but it overwhelms
the rest of the body. That spells trouble, because insulin is more than just a sugar ferry. It tells the kidneys, for example,
to hold on to salt. And more salt means hypertension. It tells cancer cells to grow, and that can mean a tumor.
Fortunately, doctors are starting to devise new ways
to treat insulin resistance--which is sometimes called "metabolic syndrome" --with drugs and lifestyle changes. They are still
working out all the connections, but already they have a list of some of the leading insulin-related illnesses:
|
 |
|
|
 |
|
|
 |
|
|
 |
 |
 |
Cancer
Insulin stimulates cell growth, and unfortunately cancer cells
have six to 10 times the number of insulin receptors--molecules that grab on to the hormone--as do normal cells. So if extra
hormone hits a pre-existing cancer cell, it makes a bad thing much, much worse. "For cancer, insulin is like pouring gasoline
on a fire," says Edward Giovannucci, who studies the epidemiology of colon cancer at the Harvard School of Public Health.
Colon, breast, endometrial, pancreatic, and prostate cancers
seem especially responsive. "We think breast cancer cells may have very special kinds of receptors, fetal insulin receptors,
that are ultrasensitive to insulin," says Pamela Goodwin, director of the Marvelle Koffler Breast Center at Mount Sinai Hospital
in Toronto. Insulin may also influence estrogen, another hormone that can trigger tumor growth. "So if you turn on one hormone,
you turn on the other," Goodwin says. She is currently testing Glucophage to see if it can lower insulin levels in breast
cancer survivors and plans to see if this affects cancer recurrence.
Cardiovascular Disease
High levels of insulin in the blood damage the lining of arteries, increase bad blood fats such
as triglycerides and LDL cholesterol, and clump blood cells together so they are more likely to block up vessels. These observations
prompted Gerald Reaven, the Stanford endocrinologist who first described insulin resistance in the 1980s, to finger the condition
for heart attacks, strokes, and cases of high blood pressure. Other research has come to back him up. A
major study by Finnish researchers in the journal Circulation followed almost 1,000 men for 22 years and found insulin
levels alone were the most powerful predictors of heart attack risk, especially in younger men. They were more powerful than
obesity levels and physical inactivity, for example. Men with the highest insulin levels had more than three times the heart
attack risk of those with the lowest. [Obese people are much more likely to have high insulin levels—jk]
The concept does have its critics. Last week in the journal Diabetes Care , Richard Kahn,
chief scientific and medical officer for the American Diabetes Association, wrote an article questioning whether the idea
of insulin resistance is truly useful, particularly when it comes to diagnosing and helping heart patients. Just calling something
by a new name, he argues, doesn't change the recommended therapies. "I don't see the value . . . especially when the treatments
are the same," says Kahn. He points out that if patients have high cholesterol, they're going to get cholesterol-lowering
drugs and advice on diet and exercise, whether or not insulin resistance is the root cause.
But other experts see value in understanding insulin's role in the clustering of cardiovascular
risk factors, particularly if it points the way toward new treatments. It's already doing that for stroke, for it's here that
one new treatment is being tested. This spring the
National Institutes of Health began a study at more than 60 research sites to see if the drug Actos, an insulin sensitizer, can reduce stroke
recurrence in certain patients.
Ovary Disease
According to the American Association of Clinical Endocrinologists,
polycystic ovary syndrome affects 1 in 10 women and is the leading cause of infertility in the United States. High levels
of insulin trigger excess production of other hormones by the ovaries, disrupting regular egg growth and menstrual cycles
and preventing pregnancy. Some of these overproduced hormones, or androgens, can also cause male-pattern hair growth on the
face and some other unpleasant appearance changes. Basically, says Mark Perloe, an Atlanta endocrinologist and polycystic
ovary syndrome specialist, "insulin is driving the ovary crazy."
Doctors now treat this ovary syndrome with insulin-sensitizing
medications like those taken by Chapman, and also recommend weight loss, which lowers insulin levels. Treatment is important
even beyond fertility problems, because untreated women with the polycystic syndrome have more than seven times the risk of
heart disease and three times the risk of diabetes of women without it.
Alzheimer's
Cells in the brain's memory and learning centers have a lot of
insulin receptors. A quick spike in insulin improves memory and performance; take insulin away, and brain function begins
to decline. But paradoxically, more insulin in the blood--insulin resistance--means less in the brain. One leading theory:
Insulin's corrosive effects on blood vessel linings gums up tiny portals in the vessels that supply the brain, making it harder
for the hormone to bring in sugar. Ultimately, this starves brain cells, suggests researcher Suzanne Craft of Veterans Administration
Puget Sound Health Care System. That could set the stage for some cases of Alzheimer's, Parkinson's, and Huntington's diseases.
Insulin also seems to clear away some beta-amyloid, a substance long implicated in Alzheimer's damage, so less of it could
cause problems.
There are, of course, many theories about Alzheimer's, and this
is far from the final word. But whatever the reason for the disease, there is preliminary evidence that getting insulin to
the brains of Alzheimer's patients improves symptoms. In Craft's recent study, a small group of Alzheimer's patients, including
Marincin, inhaled insulin. (Inhalation provides more of the hormone to the brain.) Compared with a group that only inhaled
saline solution, these patients better recalled stories and lists. It's not known, however, how long these improvements last.
Craft is now testing the insulin sensitizer Avandia in people with Alzheimer's to see if it might slow down the disease.
The tests of all these drugs may sound good, but they are far from
the only treatment--or the best--for insulin resistance. There's a lot of hope to be found around the dinner table. Most
people with resistance can actually undo it by losing as little as 5 to 20 pounds. The best eating plans, say experts, offer lots of soluble fiber, the kind found in
berries and beans and whole oats, which seems to indirectly diminish resistance, as well as lean proteins like fish. Saturated
fats may cause insulin to spike, so look for foods with healthy fats like nuts and avocados. But enjoy them in moderation.
Weight loss is important because all the risks for all the diseases associated
with insulin resistance are multiplied by obesity.
That spare tire many of us carry around the middle packs the liver in fat, and the liver responds by tossing high levels of
free fatty acids into the blood. These fats seem to block insulin from docking with its receptors on cells, increasing the
risk of starting the resistance syndrome.
Regular exercise also helps muscles better use insulin, so in
addition to her medication, Kristin Chapman works out four times a week. She also gets her heart checked every year, and has
started getting regular mammograms early, at age 35. If insulin does indeed turn on many diseases, she plans on doing her
best not to throw the switch.
SCIENTIFIC AMERICAN ARTICLE
Sept 14,2005 at http://www.sciam.com Study
Assesses Annual Cost of Obesity to Employers
Study Assesses
Annual Cost of Obesity to Employers
There are
a variety of health risks associated with obesity. The condition can be hard on the corporate wallet, too, owing to medical
expenses and missed days of work. A new study has concluded that the annual additional cost for an obese worker can reach
$2,500.
Scientists at RTI International Health, Social and Economics
Research and the Centers for Disease Control and Prevention used two data sets that encompass more than 45,000 full time workers
between the ages of 18 and 64 for the new analysis. They compared figures that included body mass index (BMI), sick days and
total medical expenditures. In general, a BMI greater than 25 is considered overweight. The researchers found that as BMI
increased, so too did medical expenses for both men and women. The additional costs ranged from $162 for slightly obese men
to an extra $1,524 for men with a BMI greater than 40. For overweight women, these costs ranged from $474 to $1,302.
When the team factored in the cost of lost work days for obese employees, they calculated that the per capita cost of obesity
amounts to between $460 and $2,485 annually.
|
|
|
|
Taking the
frequency of obesity into account, as well as the overall gender makeup of the workforce, the authors argue that for a firm
with 1,000 employees, obesity would cost about $285,000 a year. "As the prevalence and cost of obesity in the workplace continue
to increase, so does the financial motivation to search for strategies to reduce these costs," remarks study co-author Eric
Finkelstein of RTI. "Such strategies may include work site wellness and disease-management programs related to obesity." --Sarah
Graham |
|
|
|
|