|

More journal
articles on LDL’s immune functions http://healthfully.org/rl/id8.html,
http://healthfully.org/rja/id1.html, and http://healthfully.org/rja/id1.html
and review
article on infections
causing pathogenesis of atherosclerosis by
Uffre Ravnskov and Kilmer McCully
Just one of many articles show the role of LDL in the immune
system, others show the role of pathogens in atherogenesis. All this ties well
into the standard immune system
model of atherogenesis and answers three questions that the reactive products
of metabolism causation theory does not plausible answer: 1) Why are reactive
oxygen species in the
floating around in the tunic media, since the products of metabolism are within
two containers, the mitochondria and the cell walls? 2) Why does LDL get actively
transported to
the tunica media? 3) And why does
monocytes and macrophages which by design respond to pathogens, toxins, and
foreign cells, respond to slightly oxidized LDL?—jk.
http://www.jbc.org/content/258/9/5899.short
Binding and Partial Inactivation
of
Staphylococcus aureus a-Toxin by Human Plasma Low Density Lipoprotein*
THE JOURNAL OF BIOLOGICAL CHEMISTRY Vol. 258,
No. 9, Issue
of May 10, pp. 5899-5904, 1983 Printed in U. S. A.
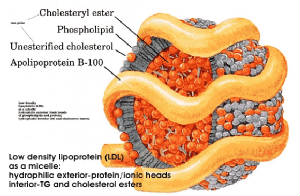
Human low density lipoprotein (LDL) in isolated
form or in unfractionated serum binds and partially inactivates Staphylococcus
aureus a-toxin. Under conditions of LDL excess, up to 90% inactivation occurs
as estimated by hemolytic titration. Inactivation is accompanied by, and
probably due to, oligomerization of 3 S native toxin molecules into 11 S
hexamers on the LDL molecules. This
process is believed to be mediated by the lipids contained in the lipoprotein.
The toxin hexamers are visualized as ring structures and stubs bound to the
spherical LDL molecules by negative staining electron microscopy. These
structures appear identical with those formed on target erythrocyte membranes
during toxin-dependent lysis. The toxin hexamers are trypsin-resistant and do
not spontaneously dissociate from the lipoprotein. The binding process appears
to be highly selective, and no similar
interaction of toxin with any other serum protein, including high density
lipoprotein [unique function of LDL as binding agent], has been observed.
LDL/a-toxin complexes exhibit some residual hemolytic activity which possibly
derives from the presence of lipoprotein-bound but nonoligomerized 3 S toxin.
This fraction of bound a toxin appears to have the capacity of dissociating
from the lipoprotein molecules and attack cells. The collective results imply a
dual role of LDL relative to S. aureus a-toxin in the organism. The lipoprotein
may exert a beneficial effect through nonimmune inactivation of a-toxin on the
one hand, but may also serve as a carrier for a small fraction of potentially cytotoxic
native toxin within the host. [Possible this is an adaption of the toxin bypass
in part the immune function of LDL].
There
are hundreds of journal
articles demonstrating that infective
agents play the key role in atherosclerosis and thus CHD (coronary heart disease).
There is strong evidence that besides transport of cholesterol and triglycerides
by HDL and LDL, they play important immune functions. This is why LDL and HDL
are present in
atheroma; there they among other things bond to, and thus disable endotoxins
produce by the pathogens in the artery walls.
The infective agents also produce a response an immune response by white
blood cells, thus their presence in the inflamed atheroma. The strong experimental
evidence thus
accounts for the presence of both white bloods cells and the lipoproteins. This
is contrary to the standard LDL theory where oxidized LDL (no mention of the
bacterial
and virus vectors or the immune role of HDL and LDL) produces an immune
response by macrophages. Since pharma
and its opinion leaders can’t refute the infection cause, they simply ignore
the issue. Pharma’s oxidation theory makes
atherosclerosis an auto-immune disease. A
much better explanation based upon experimental evidence is given by Prof. Uffe
Ravnskov in his book and journal
article of these events and the role of infective agents. In the articles below bacterial
living within
the middle layer of the artery wall trigger the immune response by T-cells
which are further aided by macrophages.
The damage caused in this process damage the arteriole (vasa vasorum)
which supply blood to the muscle cells in the artery walls. A large body of
clinical evidence (see for
examples Ignore the Awkward! by Prof.
Uffe Ravnskov—notes on this book), and also the notes on
Anthony Calpo chapter 21 The Infection Connection, from
The
great Cholesterol Con, an excellent scholarly source. --jk.
^^^^^^^^^^^^^^^^^^^^^^^^^^
http://www.ncbi.nlm.nih.gov/pubmed/23431458 J
Lipids. 2013;2013:684903 . Jan 30,2013
High-density
lipoproteins and the immune system
Abstract
High-density
lipoprotein (HDL)
plays a major role in vasodilation and in the reduction of low-density
lipoprotein (LDL) oxidation, inflammation, apoptosis, thrombosis, and
infection; however, HDL is now less functional in these roles under certain
conditions. This paper focuses on HDL, its anti-inflammation behavior, and the
mechanisms by which HDL interacts with components of the innate and adaptive
immune systems. Genome-wide association studies (GWAS) and proteomic studies
have elucidated important molecules involved in the interaction between HDL and
the immune system. An understanding of these mechanisms is expected to be
useful for the prevention and treatment of chronic inflammation due to
metabolic syndrome, atherosclerosis, or various autoimmune diseases.
From the complete version http://www.hindawi.com/journals/jl/2013/684903/
5. Conclusions
Accumulating evidence suggests that
HDL or a specific apolipoprotein associated with HDL, such as apoA-I, is involved
in the innate and adaptive immune
responses primarily through the modulation of lipid raft components in monocytes/macrophages,
dendritic cells, and T and B lymphocytes. Plasma HDL-C is usually reduced in
chronic inflammation. These findings suggest that .
However, chronic
inflammation modifies HDL from a molecule with anti-inflammatory properties to
one with pro-inflammatory properties, which leads to complex interpretation of
plasma HDL-C levels. Although recent genetic and proteomic studies have
unveiled important molecular players in HDL metabolism and immune activity, the
mechanism for HDL regulation by these molecules remains unclear. Additional
studies are required to answer several questions about HDL-C and inflammatory
disease with regard to reduced plasma HDL-C levels as potential pathogenic
cause of inflammatory diseases; HDL-C consumption and its consequences versus
benefits for protection against these diseases; and altered HDL function in
these diseases.
^^^^^^^^^^^^^^^^^^^^^^^
http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2362.2008.02031.x/abstract;jsessionid=EC115C50981171B5FF6A56394159C4FA.f02t04?deniedAccessCustomisedMessage=&userIsAuthenticated=false
European Journal of Clinical Investigation;
Volume 38, Issue 11, pages 857–862, November 2008
Multiple bacteria contribute
to intraplaque T-cell
activation in atherosclerosis
J. J. Van Der
Meer1, A. C. Van Der Wal1,
P. Teeling1, M. M. Idu2, A. Van Der Ende3 and O. J. De Boer1
Abstract
Background Infection with
microorganisms is considered a pathogenic
factor in atherogenesis. Several studies have shown the presence of a broad
spectrum of bacterial species in atherosclerotic plaques, which could trigger
local inflammation. Because T cells contribute to atherosclerotic plaque
inflammation, we studied the responsiveness of human plaque derived T-cell
cultures to bacteria of different species.
Materials and
methods Primary polyclonal T-cell cultures were generated from both
carotid endarterectomy tissue and peripheral blood of nine patients, and the
peripheral blood of eight matched controls. The in vitro proliferative
responses of the T-cell cultures against H. pylori, N. meningitidis,
N. lactamica, S. aureus, S. pneumoniae, S. epidermidis
and E. coli were analysed. T-cell proliferation was measured by 3H-thymidine
incorporation and expressed as a stimulation index. Selective outgrowth of
intraplaque microbial specific T cells was studied by calculating the ratio of
plaque T-cell SI and peripheral blood T-cell SI in each patient.
Results All patients
showed T-cell responsiveness to multiple
bacteria in their plaque tissue. Stimulation indices were in the range of
0ˇ3–30, and this degree of reactivity with the different species was
heterogeneous among patients. Selective outgrowth (plaque/peripheral blood
ratio) of T cells against multiple bacteria was observed in six out of nine
patients.
Conclusions T cells in atherosclerotic
plaques have the capacity to
selectively respond to antigens of a wide variety of microbial antigens. This
supports the view that such mechanisms could contribute to the atherosclerotic
inflammatory response.
^^^^^^^^^^^^^^^^^^^
http://journals.lww.com/co-lipidology/Abstract/2009/10000/The_role_of_hypoxia_in_atherosclerosis.9.aspx
Current Opinion in Lipidology: October 2009 -
Volume 20 - Issue 5 - p 409–414
The
role of hypoxia in atherosclerosis Hultén, Lillemor Mattsson; Levin,
Max
Abstract: Purpose of review: It is
important
to address the factors involved in the progression of atherosclerosis because
advanced atherosclerotic lesions are prone to rupture, leading to disability or
death. Hypoxic areas are known to be present in human atherosclerotic lesions,
and lesion progression is associated with the formation of lipid-loaded
macrophages and increased local inflammation. Here we summarize the role of
hypoxia in the development of advanced atherosclerotic lesions by promoting
lipid accumulation, inflammation, ATP depletion, and angiogenesis.
Recent findings: A recent study clearly demonstrated the presence
of hypoxia
in macrophage-rich regions of advanced human carotid atherosclerotic lesions.
We showed that hypoxia increases the formation of lipid droplets in macrophages
and promotes increased secretion of inflammatory mediators, and recent evidence
indicates that lipid droplets may play a role in mediating the inflammatory
response. Hypoxia also promotes lesion progression by exacerbating ATP
depletion and lactate accumulation, and the presence of hypoxia in human
carotid atherosclerotic lesions correlates with angiogenesis.
Summary: Recent studies indicate that hypoxia may play a key role
in the
progression to advanced lesions by promoting lipid accumulation, increased
inflammation, ATP depletion, and angiogenesis. Further understanding of the
effects of hypoxia in atherosclerotic lesions could indicate potential
therapeutic targets.
^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^
http://informahealthcare.com/doi/abs/10.3109/07853890.2010.497767
September 2010, Vol. 42, No. 6 , Pages 394-403
(doi:10.3109/07853890.2010.497767) University of Birmingham Centre for
Cardiovascular Sciences
The role of monocytes
in atherosclerotic coronary artery disease
Abstract: Inflammation plays a key role in
the pathogenesis of atherosclerosis. The more we discover about the molecular
pathways involved in atherosclerosis, the more we perceive the importance of
monocytes in this process. Circulating monocytes are components of innate
immunity, and many pro-inflammatory cytokines and adhesion molecules facilitate
their adhesion and migration to the vascular endothelial wall. In addition to
the accumulation of lipids and formation of atherogenic ‘foam’ cells, monocytes
may promote atherosclerotic plaque growth by production of inflammatory cytokines,
matrix metalloproteinases, and reactive oxidative species. However, the
contribution of monocytes to atherogenesis is not only limited to tissue
destruction. Monocyte subsets are also involved in intraplaque angiogenesis and
tissue reparative processes.
The aim of this overview is to discuss the
mechanisms of monocyte
activation, the pivotal role and importance of activated monocytes in
atherosclerotic coronary artery disease, their implication in the development
of acute coronary events, and their potential in cardiovascular reparative
processes such angiogenesis.
^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^
http://link.springer.com/article/10.1007/s12350-010-9263-x#page-3;
ALSO pdf
http://download.springer.com/static/pdf/676/art%253A10.1007%252Fs12350-010-9263-x.pdf?auth66=1414730536_909f4c5f3727da727a6c3247ea617561&ext=.pdf
Journal of Nuclear cardiology, Sept/Oct 2010
Molecular
imaging of inflammation and intraplaque vasa vasorum: A step forward to identification
of
vulnerable plaques?
Current developments in cardiovascular
biology and imaging
enable the noninvasive molecular evaluation of atherosclerotic vascular disease. Intraplaque neovascularization sprouting from
the adventitial vasa vasorum has been identified as an independent predictor of
intraplaque hemorrhage and plaque rupture.
These intraplaque vasa vasorum result from angiogenesis and most likely
under influence of hypoxic [lack of oxygen] and inflammatory stimuli. [Then
goes on to describe imaging techniques.]
Pathophysiology of the Vulnerable
Plaque: Traditionally, the burden of
atherosclerotic disease was estimated from the percentage of stenosis detected
by angiography. However, it has
become
apparent [2 decades ago] plaque rupture and consequent cardiovascular events
are dependent on the plaque composition rather than stenosis.
Analyses of culprit lesions demonstrated that
plaque vulnerable to rupture are characterized by active inflammation, a large
lipid core with a thin fibrous cap, positive remodeling, intraplaque
hemorrhage, and intraplaque neovascularization of the vasa vasorum.
Inflammation: Inflammation is one of the hallmarks of
plaque vulnerability. Macrophages are the most prevalent inflammatory cell in
the atherosclerotic plaque and play a major role in the pathophysiology of
plaque vulnerability. Macrophages
secrete proteolytic enzymes, which degrade the extracellular matrix weakening
the fibrotic cap structure and ultimately leading to plaque rupture.
Vasa Vasorum Neovascularization: Interruption
of the adventitial vasa vasorum
results in media necrosis, showing they are critical for
nourishment of the media. The vasa
vasorum are unevenly distributed along the vessel wall. It has been hypothesized that areas of low
vasa vasorum density have less efflux of lipoproteins and are prone to
inflammation. A relative hypoxic
state…
may be the trigger for the formation of atherosclerotic plaque.
This hypothesis has been supported by the
presence of hypoxic [lack of oxygen] and inflammatory factors….
Clinical
applications:
Due to the tortuous and ever moving nature of the coronary arteries,
imaging of coronary atherosclerotic plaques is a major challenge…. Because
atherosclerosis is a systemic inflammatory disease and local changes in
macrophage content and vasa vasorum density are often uniformly present in
different vascular beds, the presence and composition of atherosclerotic
plaques in peripheral arteries can be used as an indication for atherosclerotic
disease of the coronary arteries.
^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^
http://jid.oxfordjournals.org/content/180/3/780.short J Infect Dis. (1999) 180 (3): 780-790.
Cellular
Oxidation of Low-Density Lipoprotein by Chlamydia
pneumoniae
Abstract: A spectrum of clinical and
epidemiologic studies implicate infectious agents, including Chlamydia
pneumoniae, in the pathogenesis of atherosclerosis. The complexity of
atherosclerotic disease necessitates examining the role of infection in the
context of defined risk factors, such as high levels of native low-density
lipoprotein (LDL). Although native LDL does
not have atherogenic properties,
cellular oxidation of LDL alters the lipoprotein into a highly atherogenic
form. In
this report, C. pneumoniae and
chlamydial hsp60, an inflammatory antigen that was recently localized to
atheromas, were found to induce cellular oxidation of LDL. These data provide
initial evidence that an infectious agent can render LDL atherogenic and
suggest a mechanism whereby C. pneumoniae may promote atheroma
development. ^^^^^^^^^^^^^^^^^^^^
In one of the 2 best scholarly books
on the cholesterol myth, all the important related topics are set out in length. (The
other is Ignore
the Award, Prof. Uffe Ravnskov, 2010, a shorter work). Both cover
the real major cause of CVD, infectious agents within the
artery walls. Below are experts from The Great Cholesterol Con,
Anthony Colpo, 2006
Chapter 21:
The Infection Connection. A
rapidly-expanding volume of research is implicating common infectious agents—including
the respiratory but Chlamydia pneumoniae,
the ulcer-causing Helicobacter pylori
bacteria, herpes viruses such as cytomegalovirus, and Herpes simplex and even
dental infections—as playing a direct role
in the instigation and progression of CHD…. A review of thirteen published
studies in which researchers went hunting for the organism [Chlamydia pneumonia]
in arterial tissues showed that the organism could be detected in over half of
all atheromas, but in only 5 percent of adjacent, lesion-free arterial tissue
samples 207-208…. [e]xamined fifty human atheroma specimens, they found that
forty-four percent were positive for one or more strains of periodontal
bacteria, 2008. Another potentially
confounding factor is the
fact that total infectious burden… not just the presence of any single bacteria
or virus. In a representative study, 233
patients at a Washington DC cardiovascular research unit underwent coronary
angiography to determine the presence of coronary artery disease, then were
tested for a variety of bacterial and viral antibodies. The prevalence of CAD
was 48, 69, and 85
percent in individuals with antibodies to two or less pathogens, to three or
four pathogens, and to five pathogens, respectively, 210. There
is now compelling evidence to show that low cholesterol levels increase the
susceptibility to infectious disease, while high cholesterol levels appear to
protect against infection!... The cell membranes of gram-negative organisms
contain what is known as endotoxins,
or lipopolysaccharide (LPS), while Gram-positive microbes contain lipoteichoic acid
(LTA). LPS and LTA are virulent factors
that trigger the inflammatory response and cause much of the unpleasant
symptoms of infection. In the laboratory
experiments, LPS and LTA rapidly bind to and are subsequently inactivated by
HDL and /or LDL (36-39). In additions Staphylococcus
aureus alpha-toxin, a
toxin produced by most strains of Gram-positive Staphylococcus bacteria that causes
damage to a wide variety of
cells, is bound and almost totally inactivated by LDL, 211. In men with high
cholesterol, mononuclear cells
(lymphocytes and monocytes) exerted a far more robust immune response than
those in men with lower cholesterol level…. 68,400 deaths, found that as total
cholesterol went down, mortality from respiratory and gastro-intestinal
diseases—most of which are initiated by infectious organisms—went up, 212.
|
|
The
Great Cholesterol Con, Anthony Colpo, 2006, Chapter 21, The Infection
Connection, excerpts by jk.
Chapter 21: The Infection Connection. A rapidly-expanding volume of research is
implicating common infectious agents—including the respiratory but Chlamydia
pneumoniae, the ulcer-causing Helicobacter pylori bacteria, herpes
viruses such as cytomegalovirus, and Herpes
simplex and even dental infections—as playing a direct role in the
instigation and progression of CHD…. A review of thirteen published studies in
which researchers went hunting for the organism [Chlamydia pneumonia] in
arterial tissues showed that the organism could be detected in over half of all
atheromas, but in only 5 percent of adjacent, lesion-free arterial tissue
samples 207-208…. [e]xamined fifty human atheroma specimens, they found that
forty-four percent were positive for one or more strains of periodontal
bacteria, 2008. Another potentially
confounding factor is the fact that total infectious burden… not just the
presence of any single bacteria or virus.
In a representative study, 233 patients at a Washington DC
cardiovascular research unit underwent coronary angiography to determine the
presence of coronary artery disease; then were tested for a variety of
bacterial and viral antibodies. The
prevalence of CAD was 48, 69, and 85 percent in individuals with antibodies to
two or less pathogens, to three or four pathogens, and to five pathogens,
respectively, 210. There is now
compelling evidence to show that low cholesterol levels increase the
susceptibility to infectious disease, while high cholesterol levels appear to
protect against infection!... The cell membranes of gram-negative organisms
contain what is known as endotoxins,
or lipopolysaccharide (LPS), while Gram-positive microbes contain lipoteichoic acid (LTA). LPS and
LTA are virulent factors that trigger the inflammatory response and cause much
of the unpleasant symptoms of infection.
In the laboratory experiments, LPS and LTA rapidly bind to and are
subsequently inactivated by HDL and /or LDL (36-39). In additions Staphylococcus aureus alpha-toxin, a toxin produced by most strains
of Gram-positive Staphylococcus
bacteria that causes damage to a wide variety of cells, is bound and almost
totally inactivated by LDL, 211. In men
with high cholesterol, mononuclear cells (lymphocytes and monocytes) exerted a
far more robust immune response than those in men with lower cholesterol
level…. 68,400 deaths, found that as total cholesterol went down, mortality
from respiratory and gastro-intestinal diseases—most of which are initiated by
infectious organisms—went up, 212.
|