 |
|
recommended longer
|
|
Cancer basics and chemotherapy
|
 |
 |
|
For
a concise covering of cancer.
I have rewritten the section on cancer based up discovering that cancer is dependent upon glucose, and therefore
can be starved into remission or better. Sadly, though I have been reading the technical journals and summation articles
I hadn't discovered the Warburg Theory (1924) until 2016. The science is solid; I have spent 6 months examining it.
As a consequence I have rewritten one of my 2 summation articles on cancer and its dietary fix. What follows
is that work. I have left my older work up, much of its is valid. I simply didn't want to spend the time
on rewriting both. I have other trees to chop.
^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^
This
applies to 95% of all cancer patient, that chemotherapy cannot alter
significantly the course of the disease--a few cancers it can.
^^^^^^^^^^^
CANCER basics & CHEMOTHERAPY- 11 pgs –
1/13/17 http://healthfully.org/rc/id16.html
& long version rl/id4
Complying with laws, below
reflects my views and is not a recommendation for others to follow.
Key
points: Moved to
NT-Summation-cancer-diet-fasting in diet > KD diet.
That
all cancers have defective metabolisms because of mutations in their
mitochondria.
While
each cancer is unique, the norm is for the mitochondria to have lost the
ability to metabolize fat and to metabolize glucose aerobically; via., the
mitochondria make ATP by a fermentation process.
Without
ATP cells soon die, thus cutting off glucose by dietary restriction will kill
cancer
Since
there are minor secondary sources of energy such as glutamine, the cancer will
likely shrink due to apoptosis and become dormant thus requiring a life-long
ketogenic diet.
An
indolent cancer becomes metastatic because of fusion of their mitochondria to a
microphage.
Because
of damage to the immune system and side effects, I would forgo all
chemotherapies that can’t cure.
I
would use fasting and ketogenic diet prior to excision (at least 2 weeks of
fasting prior).
I
would use diet and fasting for all cancers, reliance upon which depends on
initially findings and lab reports on the tumor: A likely metastatic neoplasm,
even if local,
such as small cell lung, requires maximum dietary treatment, a cancerous polyp
removed from the colon minimal.
[If
the cancer is stage I-III, excision is sufficient unless there is a significant
chance to there being distant clumps of cells (metastatic cells) such as with
small cell lung cancer.[1] Therefore, I would forgo for stage I-III
chemotherapy, unless in clinical trials it can produce a cure in over 30% of
metastatic cancers.]
There
is a reason why the war on cancer, started under President Nixon has very few
bright spots, though of course pharma claims much more. Maximizing profits is
at conflict with
understanding the disease. Preventing it, and when that fails curing it. It
is essential to understand the inroads
made upon medical science by corporate medicine: Corporate medicine is market
driven; medical science evidence driven.
These two approaches result in different explanations concerning cancer.
The goal here is to understand the
general basic biology of cancer, and then its treatment options based quality
scientific evidence—without market considerations. What follows is based
upon sound science with
sources. Marketing science is driven by
profits, & thus promotes aggressive drug cocktail for everyone with
cancer. Prevent is given deceptive lip
service. With a couple exception,
chemotherapy does more harm than good. Pharma’s
marketing ploys confirms Harvard
Prof. Dr. Marcia Angell’s observation that we have
“the worst system we
could imagine.” To learn more read Marketing Science & Side Effects, and you will learn how doctors are taught by Pharma
to be
pill pushers, and why they are.
It is as Prof. Goldacre writes: A
perverse system produces perverse results.
“A benign
tumor is a mass of cells (tumor)
that lacks the ability to invade
neighboring tissues or metastasize.
These characteristics are required for a tumor to be defined as cancerous and
therefore benign tumors are
non-cancerous. Also, benign tumors
generally have a slower growth rate than malignant tumors and the tumor cells
are usually more differentiated (cells have normal features). Benign tumors are typically
surrounded by an outer surface (fibrous sheath of connective
tissue) or remain with the epithelium. Common
examples of
benign tumors include moles,
colon polyps,[2]
and uterine
fibroids.
Although benign
tumors will not metastasize or locally invade tissues, some types may still
produce negative health effects…. [Some types of] benign tumors can become
malignant…. invade adjacent tissues or spread to
distant sites by metastasizing. For
this reason, benign tumors are not classed as cancer”
Wiki.
Bad pharma has blurred the distinction
between benign and
malignant by calling benign tumors “carcinoma”, then aggressively treat with
surgery and chemotherapy. Critics point
out in journal articles the negative consequences of treating benign (small
local) tumors of the breast prostate, thyroid cancers, and others tissues with
adjunct chemotherapy following excision. Yet pharma ignores this and through
their KOLs (Key Opinion Leaders) sets up guidelines for aggressive treatment
which includes chemotherapy. Their KOLs write medical textbooks, run the
clinical trials, and instruct physicians in mandated continuing education
classes. In this and other ways pharma
shapes the practice of medicine. One
ways is that on an average over half the revenues in a cancer clinic is derived
from the spread of the cost of a drug and what they receive for administering
it in their office. This topic is
covered at Cancer long version and in the Journal of the British Medical Association,
Nov. 2016, Cancer Drugs, Survival and Ethics. This link is to a sampling of articles in leading journals on bad pharma.
With regulatory capture, the FDA often
grants patents to drugs that are not in the best interest of the patient. Moreover
pharma’s role in the production of
journal articles entails bias. For
Industry funded trials positive
bias averaged 32% (range 11 to 69%) for clinical trials
based on a comparison
of the raw data submitted to the FDA to the journal articles. And it is worse,
FDA approval is flawed. Surrogate endpoints of shrinkage of tumor
and/or duration in which tumor doesn’t grow are used by the NIH in a very
select population of terminal patients (younger patients who have not undergone
prior chemotherapy). Unfortunately those
with no treatment if they have more than a year to live would do better than
the chemo cohort. This is because the
cancer cells that have thrived during the chemo, now that the frail cells have
been eliminated, are getting all the energy molecule glucose and tumors are
very glucose hungry, up to 200 times more than a normal tissue--to be explained
later. Moreover, the quality of life is
reduced based upon the often horrendous side effects. And it gets worse, for
it is the norm to use
the chemo on those without metastatic cancer, and depending on type most have
been cured by excision, thus no benefit from chemo. More on this later under
Hope’s Hypothesis. Typically in those with terminal cancer it
translates into an average life extension of 1 to 3 months—general the duration
of the chemo therapy. Once stopped the vigorous
remaining tumors cells resume growing. Not
surprisingly, a 2015 study Published in the BMJ (one of the 5 top English
medical journals) found that most cancer drugs in the real world population “do
not increase survival”, at. And
it gets worse, industry
funded studies are always biased in favor of industry. A study which relied upon the raw data found all 74 clinical
trials journal
articles industry produced were biased; its average 32%. It as Prof. Goldacre
said, “The devil is in the details.”
This makes good advice and informed
decision unlikely.
“Cancer (malignant neoplasm) is a broad
spectrum of diseases involving improperly regulated cell growth. For that cell
growth to become
life-threatening it must be capable of sufficient reproduction so as to disrupt
essential bodily processes. Over 80% of
fatal cancers spread to more distant part of the body through the lymphatic or
blood systems—some such as cerebral cancer destroy a vital organ, and others
such as liver, and pancreatic simply
grow beyond the margins of the tissue into other organs. With the exception
of blood and lymphatic
cancers, they form hard tumors. One of the most important factors in classifying
a tumor as
benign or malignant is its invasive potential” Wiki.
A microscopic examination of a biopsy by
itself is insufficient to prove that the
tissue is malignant, for it doesn’t reveal the properties of being invasive
and/or metastatic. Lab reports often
numerical grade the tissue based on shape of cells, the heterogeneity of cells
in tumor to produce a probability rating.
Lab write up of a biopsy very often use cancerous and carcinoma though
it should be prefixed with an adjective such as likely or unlike. Cancerous
can only be definitively determined
with additional imagining, such as MRI and CAT scan. Depending on lab findings,
removal often is
the best choice, and but subsequent chemotherapy often isn’t necessary.
Oncogenesis (carcinogenesis): literally
the creation of cancer. It is a
process by
which normal cells are transformed
into cancer cells. According to the standard theory (which I no-longer hold),
“there is a progression of changes at the cellular genetic and epigenetic [regulate
the expression of other genes] that ultimately reprogram a cell to undergo uncontrolled cell
division,
thus forming a malignant mass. Over 98%
of potential mutations and epi-mutations will have no bearing on cancer” Wiki. There are 3 theories of how a tumor becomes
malignant (invasive). It is important
for me to understand which theory fits best the evidence, and also how cancers
produce the energy molecule ATP, for as you shall see, it affects my treatment
choices.
Three theories on
conversion of a tumor into cancer: Standard theory is that there are typically
seven essential types of mutations such as the cell line becoming immortal,
fooling the immune system, etc. necessary to convert a benign tumor. The second
theory is that the tumor signals
stem cells to become involved, and they give the tumor cells the properties
needed to become cancerous. The third is
similar but having the changes brought about by M2 macrophages. It seems that
the only essential mutation for
a cancer occurs in the mitochondria, known as the Warburg
Hypothesis (1924
observation) which limits the metabolism of glucose in the mitochondria to
fermentation (anaerobic). This I will
develop at the end since it entails way to starve cancer by having the body
switch to fat metabolism—now lacking in cancer cells. Yes, starve cancer!
A) Six-mutation theory: This is the theory favored by pharma (and once I too with the
aid of stem cells until Dec. 2016).
It holds that 6 mutations are necessary for a tumor to become invasive,
and these gradually accumulate among the many other mutations in the cell’s
nucleus DNA (see Scientific American, July 2003) . The theory holds that random
mutation, whose
rate is increased through exposure to mutagenic substance, radiation, or other
forms of stress, and/or if a gene which checks the reduction of DNA during
mitosis is switched off or damaged, such as the P53, BRAC1, or BRAC2
genes—being the best known and studied.
Common mutations it is held as causes (1) the cell to replicate at a
high rate, (2) fail to respond to signals to return to the normal rate, (3)
evasion of apoptosis signals (programmed
cell dismantling), (4) angiogenesis (causing new blood vessel to nourish the
expanding tumor, (5) to reproduce bypass the telomerase system which limits
replication to about 50 division, (6) not appear as foreign to immune cells
when the tumor cells break off and invade different tissue type and/or migrate
to distant locations using the lymph or blood circulatory systems for
transport. To this, I would add is the
ability to penetrate membranes which form barriers. This explanation ignores
other essential
changes in a cancer: (1) the loss of the
ability for aerobic metabolism of glucose using an inefficient system producing
lactate anaerobic fermentation, (2) deformed mitochondria (the vacuoles engines
produce over 90 of the ATP used by the body for energy) being deformed, (4) the
inability to metabolize fatty acids (fats) (3) the involvement of the
mitochondria. of For most tissues, 7 or
more mutations are required to create a malignant tumor. Less than 10% of all
cancers involve
inherited mutations, the remainder is a result of environmental factors and bad
luck. Over half the cancers are
attributable to carcinogens. Excluding
skin cancer, only about half of all cancers prove fatal.
B) Role of Stem cells
theory: A way to explain the properties of a cancer
without so many mutations. There must be
some, otherwise there wouldn’t be a benign tumors consisting of what once was
normal cells. Most significant are
mutations that diminish the ability of cells to produce an exact copy of the
parent cell DNA. This increases the
lineage’s number of mutation typically about 10 fold. In the stem-cell
theory, stem cells in their
reproductive-healing role then step in to convert some of the tumor’s benign
cells to cancerous cells. An April 2006 article in Scientific American and another in July (also at) claimed that stem cells were what was turning a
cancer into metastatic phase.[3] On stem cells Wiki:
“they are
undifferentiated
biological
cells,
that can differentiate into specialized
cells and can divide through mitosis to produce
more
stem cells, which are found in various tissues.
In adult organisms, stem cells and progenitor
cells act as a repair system for the body, replenishing
adult tissues. Stem cells maintain
the normal turnover of regenerative organs, such as blood, skin, or intestinal
tissues. Stem cells possess two
properties: self-renewal (to maintain
through cell division the undifferentiated
state) and potency (to give rise to
any mature cell type). Induced pluripotent,
these are not
adult stem cells, but rather adult cells
(e.g. epithelial cells) reprogrammed to give rise to pluripotent capabilities
of forming more than one type of tissue.
A progenitor
cell is a biological
cell that, like a stem
cell, has a tendency
to differentiate into a specific type of cell, but is already more specific
than a stem cell and is pushed to differentiate into its "target"
cell… and can divide only a limited number of times.” The occasional
finding of stem cells in
malignant tumors, and the heterogeneity of cells in most malignant tumors is
held to demonstrates their role: it fit
the evidence; but a neat theory was shot down by facts, some below.
C)
Role
of type tumor associated macrophages[4] (TAM): This is similar to the stem-cell hypothesis
only the role is filled by macrophages; the supporting evidence is strongest
(the extent of this evidence is to be found at a review journal article link to my
published version, on line, and summarized 2012 Allevena. “Contrary to expectations, in
malignancies, tumour-associated
macrophages (TAM) promote disease progression by supporting
cancer cell survival, proliferation and invasion.
TAM and related myeloid cells…. also promote tumour angiogenesis and suppress
adaptive immune responses. Dr. Seyfried in his lecture
points that experiments show that the DNA from the nucleus of cancer isn’t the
cause of the cancer, but rather the mutations in the mitochondria which cause
inefficient glucose metabolism. In experiments by inserting the mitochondria of
a cancer cell into a normal cell, that cell will become cancerous—a event that
won’t happen if the DNA of the cancerous cell is inserted. Macrophages
which are immune cells which
engulf foreign substances including bacteria and viruses, help dispose of the
products of cell apoptosis, and stimulate the growth of new tissue in the
repair process on very rare occasions will attach to a tumor and acquire the
defective mitochondria of the cancerous tumor.
This will turn the macrophage into a cancer cell. “In established
tumours, TAM resemble M2-like macrophages… in the context of a growing tumour they may
favour disease progression. [42,50–54]. Cancer-related
inflammation is now recognized as a hallmark
of cancer [55,56]. Macrophages
are key initiators of the subtle chronic
inflammation present in the tumour microenvironment, as they are major
producers of inflammatory mediators. IL-6 is a key growth-regulating and anti-apoptotic
cytokine, having tumour-inducing activities on both malignant and stromal cells. In mouse
models of colitis, IL-6 is produced mainly by macrophages in response to
intestinal injury and in an NF-kB-dependent manner.
Tumour
cells exploit the ECM degradation mediated by TAM to
invade locally, penetrate into vessels and disseminate to give distant
metastasis. The chemokine CCL18 produced by
TAM has been shown recently to play a critical role in promoting breast cancer
invasiveness by activating tumour cell adherence to ECM. Tumour macrophages have the ability
to suppress the adaptive
immune response, thus contributing directly to the phenomenon of immune evasion
of cancer. in the majority of human tumours
high numbers of infiltrating TAM have been associated significantly with
advanced tumours and poor patient prognosis [11,15,42,111], TAM are
present in large numbers in tumour
tissues and are key promoters of cancer-related inflammation.” Summary article 2012 Supra. The six mutation theory and the role
of stem cells fall far
short in evidence to TAM.
On treatment
and
prognosis is about the typical, common cancers
For the 5 common
cancers (lung, colorectal, breast, prostate &
pancreatic), 3 of them if assumed not metastatic on initial diagnosis can be
successfully be treated by excision (over 70% at 10 years will not have died
from that cancer). Two of them small
cell lung cancer (the most common type) and prostate over 90% die in the first
2 years. Pancreatic cancer is locally
invasive and cannot be entirely removed by surgery, and small cell lung cancer
has metastasized by the time it can be seen with imaging. For each there type
of cancer there is a bell
curve of variation for rate of growth.
Rate of growth can only be determined on subsequent imaging.
FIVE KEY FACTORS AFFECTING
PROGNOSIS (the benign tumor that a TAM has converted into a cancer:
One factor is the
stage I-IV, which is based upon the degree of
invasiveness of the cell line and size of cancer. A larger tumor, spread to
adjacent tissue, or is found in lymph nodes is more likely to have undergone
the changes involving TAM and become metastatic (lethal). For an example 5-year survival of breast cancer, if
greater than 5 cm 65%, for less than 2 cm 96%—tissue of origin makes only a
small difference. Each tissue type
percentage figures is different. How fast the cancer invades adjacent tissue
and spreading through the tissue of origin can only be determined by a successive
examinations months apart. Second,
is the primary tissue. Each tissue has its own prognosis. Pancreas has 3 common primary tissues;
however, all tissues produce a very high percentage of aggressive malignancies
(the 5-year survival rate is 2%). The third
is the variation in cells within
the tumor the more likely a M2 obtained a mitochondria from the tumor that will
cause the mitochondria to become caner.
And if it still is mutating at a higher, the less like that all the
cancer sell will be removed or respond to dietary restriction or
radiation. Fourth is the degree
of differentiation from the tissue of
origin. The closer the tumor resembles
the parent tissue the more likely is it that it won’t be cancerous or if
cancerous will be indolent and thus easy to cure with excision and diet. The
complex processes involving many genes,
their control mechanism, the also way the M2 macrophages (TAM) and other immune
cells respond to the benign and later malignant tumors, all this makes each
cancer unique. Fifth, the presences
and involvement of M2 macrophages. But for a few experimental settings, the
lack
of awareness entails that lab reports don’t contain this information.
On Staging: While the stage of cancer development
is important as to survival (success of excision in curing cancer) the early
detection yields no survival benefit.
Yes finding a cancer early doesn’t improve the patient’s chances versus
findi later. Theory behind early
detection is that the clock is running, and at some point the cancer will have
a mutation that will allow to spread to distant tissues. Allow me to explain,
if it is really a cancer,
not a benign in situ tumor, then by the time it has gone invaded other tissues,
it has already done a fusion with a macrophage, and what properties that tumor
has gained have determined it properties; viz., weather the cancer is deadly or
not. So removing a pea size tumor is
already too late if mitochondria fusion has occurred. Only a certain percentage
of fusions are deadly,
and that percentage is determined by the tissue type. Some tissues have most
of the cancers
progress slowly while others like small cell lung tissue are very likely
metastatic rapid growth. This theory of early detection was shot down in the
fifties when a program of screen with X-rays was adopted. Since death typically
occurs within 9 months, answers to this question was in hand by the end of the
second year. The program was stopped
because there wasn’t a statistically significant benefit. It was in an
era when most trials were ran by
a university, even those funded by pharma, their further involvement was
minimal. That has all changed with the
changes made by the Republicans during Reagan’s administration. Others
like breast cancers are in between. Thus a so called breast cancer of 2 cm or
less has only a 4% chance of killing the woman; while one of 5 cm has a 35%
chance. The point is that with a regular
checkup only 11% of the metastatic cancers haven’t progressed from small to 5
cm. Some of those are indolent and the
new colonies will take years to show up, but most aren’t. Early discovery
doesn’t change the nature of
the cancer. This has again been
confirmed with breast cancer. The harm
done by early detection, treating tumors that aren’t cancer. In a study
published in 2017 in the BMJ,
article drawing attention to the article published in the Annals of internal
Medicine found that one in 3 women was over-diagnosed (a polite way of saying
they didn’t have cancer, just a benign tumor). “Seventeen
years of organised breast screening in Denmark has not reduced the incidence of
advanced tumours but has markedly increased the incidence of non-advanced tumours
[not cancer] and
ductal carcinoma in situ” BMJ, 2017. This is the same for other
detection methods which
lead to a biopsy. I was diagnosed with
prostate cancer based on a biopsy in 2006, and didn’t go back for further
screening after reading the lab report which call it “carcinoma”. The
percentages were the same for biopsy
following a high PSA as for mammogram.
Millions have had their lives shortened by treating a phantom
cancer: they poison called chemotherapy,
made all the worse by chemical castration (block estradiol or testosterone). But
pharma who miss-educates doctors
benefits.
FOUR KEY PROBLEMS WITH MOST
CHEMOTHERAPIES, LACK OF SELECTIVITY, DEPRESSION OF IMMUNE SYSTEM, SUMPRESSION
OF TUMOR GROWTH SHORT-TERM DOES NOT PRODUCE A CURE, DEVELOPMENT OF RESISTANCE
AND ELIMINATION OF WEAKER MALIGNANT CELLS: 1) Cancer cells are nearly identically
to body cell; their genes and thus proteins are identical. Thus unless the tissue
type can be eliminated
without dire consequences (as with testicular cancer) it is unlikely that the
chemo will produce a cure. Thus very few
chemotherapies harm only cancerous tissues. 2)
The common cancer drugs
function by blocking functions vital to cells and tissues (and thus the
patient) such as the production of new blood vessels, cellular reproduction, etc. “Thus
chemotherapy also harms normal cells especially those that divide rapidly, most
notably in the bone
marrow, digestive
tract, and hair
follicles.
This results in the most common
side-effects of chemotherapy: myelo-suppression (decreased
production of blood cells, hence also immuno-suppression),
mucositis (inflammation of the lining of the digestive tract), and alopecia (hair loss). Virtually all chemotherapeutic regimens can
cause depression of the immune system, often by
paralysing the bone
marrow and leading to a
decrease of white
blood cells, red
blood cells, and platelets” Wiki.
Thus since macrophages have vital functions to develop a chemo to
suppress their functions would soon prove fatal. This explains why chemo
therapies (with a
few exceptions) can be given only short term, and often not continuously but
every week or two for a couple of months.
3) The surrogate endpoint of
tumor shrinkage and progress-free period is used by the FDA for drug
approval. This is a very low hurdle that
can extend the life of a terminal patient near death a few weeks or months, but
doesn’t translate into benefit for patients whose death from cancer is a year
or more out, or who were cured by surgery.[5] Causing damage throughout the body is why
most chemotherapies are given only short term intermittently (such as biweekly)
and stopped after a couple of months.
They at best for the terminal patient near death prolongs life on average
2 months for metastatic cancers.[6] This explains why there is a lack of
long-term studies with the end point of death for those with stage I, III, and
III cancers.[7] And if stage IV, I wouldn’t want to have the
decline of my health in my last few months.
4) If the chemo proves toxic
to the weaker malignant cells, those that survive are both resistant to the
chemo, and now are not competing with the weaker tumor cells for the limited
supply of glucose, their energy molecule.
Thus once the chemo has stopped the malignant cell typically then
reproduce at an accelerated rate.
Moreover since the immune system often plays a key role in suppressing a
cancer, to weaken the immune system for many also contributes to the growth and
spread of the cancer. If I was likely to
be cured by excision or radiation, the use of chemo subsequent or prior is a
choice I would never make--see Hope’s
hypothesis below. A
recent of new drugs (2003 to 2013) showed them on an average no better than old
drugs at Jan 4, 2017. Of course pharma exaggerates the
benefits and downplays the side effects.
Evolution works for the
survival of the most vigorous cancer cells. This is why
in most cases when a cancer returns the same treatment is not repeated, or if
repeated has little positive effect. The
very high rate of mutation for most aggressive cancer gives an evolutionary
resistance that entails survival of some of the cells during chemotherapy. (That
is why the greater the variation in
appearance seen under a microscope of the tumor cells is associated with an
increased risk of the cancer proving to be metastatic.) Thus for a chemotherapy
that reduces tumor
size, some of the cells will survive, and continue to reproduce. “Those
resistant cells reproduce at the
highest rate will make up most of the new tumor.… Over a sufficiently long
period of time there always are metastases that share little with their tumor
of origin…. But the sad reality is that the current cure rates for
metastatic-disease still sit where they have been throughout the history of
humankind—in a neighborhood near zero” (Slipping Past Cancer’s Barriers, Mauro
Ferrari, American Scientist, Vol. 101, p. 430 12/2013). These three issues entail
that for nearly all
chemotherapies entail the net result is not in the best interest of the
patient.
THE PROBLEM OF DESTROYING CELLS THAT
HAVE
ALL OF THAT PERSON’S GENES: A metastatic cancer is as stated a line of
cells from a
person’s body that have undergone mutations in the mitochondria the result of
reactive chemical the products of metabolism and glycation that disables its
ability to metabolize fats and glucose aerobically. (Mitochondria have their
own genes.) The macrophages in a rare fusion process
acquire the abnormal mitochondria with its genes to become cancerous. Instead
of growth of lung tissue to repair
damage from an accident or infection, the mitochondria now function like
aberrant lung tissue. This cancer is
from that person’s body cells with all its genes. How can a chemical destroy
those body cells
without also destroy other lung cells, or other tissue throughout the
body? It can’t. Consider how different
a bacteria is or the protozoan Malaria
from human cells, different in many ways, yet there isn’t for Malaria a
chemotherapy that will destroy the disease.
And with bacteria, the antibiotics must be given in low dose so as not
to kill the patient. The antibiotic only
helps the immune system destroy the bacteria generally by slowing the
reproduction of the bacteria. Once the
immune system is damaged by chemotherapy, survival is shortened if the cancer
turns out NOT to be metastatic, or
if metastatic and indolent. How much is
a guess because population data banks are not open to the academic community;
these include records by major insurers and hospital chains such as Kaiser, and
by our government (Veterans Hospitals). Informed consent requires the patient
and being given valid figures on the endpoint results of all causes of death
and side effect in a real world population, and his oncologist needs access to
these figures for giving advice. But
pharma, the global trillion dollar gorilla is very good at market.
What of cancer cells
which no longer are held in check by white blood cells, as they once were
before TAM modified it in a way that permits the cancer cells to spread to
distant tissues. The chemo must somehow
destroy the cancer without now the aid of the white blood cells; it can’t. Oncologist
use the term “survival” to sell patients on a poison that for most
chemotherapies extends life of a terminal patient under 3 months; that is not
“survival”, only modest extension of the patient’s suffering. The
poison is used short term because if it
is used continuously it will kill the patient.
And even short term, most patients have a major reduction in the quality
of life. If oncologist weren’t merchants
of false hope, and patients knew the meaning of their use of “survival”, most
would refuse chemotherapy.
SHOULD CHEMOTHERAPY BE
GIVEN TO A STAGE I, II, OR III CANCER? Typical 5 year survival
for breast cancer is 97%
for stage I, 85% for stage II, and 65%
for stage III.[8] (The very higher survival rate for stage 1
comes from treating many benign tumors, called malignant). If chemotherapy is given to those who will
remain cancer free, it is life shortening and affects quality of life. This
negative effect is very significant in
cancers of the prostate and breast because of hormone blocking (castrating)
drugs are included in the chemotherapy. Yes,
sex hormones not only increase libido, but also promote health, which is why
pharma and the NIH do tobacco science to claim the opposite (see Natural HRT and Testosterone links). Without estrogen, total morality was double at 10 years. Moreover, if the surgery misses some of the
cancer, the chemo won’t destroy that tumor.
Once observed it can be removed.
If the cancer has evolved to be metastatic in the interim period, it
would have with or without the chemo.
Chemo, since it can’t destroy the missed tumor it doesn’t change the
course of events. Thus for stage III
breast cancer (cancer found in nearby lymph nodes), 65% of patients must endure
chemotherapy when they don’t need it and its horrible side effects, which
persist for years for about 40%. And for the 35% who will die of cancer, they
are gaining nothing but side effects.
Since they are not near death, the cancer is more likely to be more
aggressive now that the febrile tumor cells have been eliminated, and all the
glucose absorbed is used by the surviving cells. Rather than treat every one,
it would be
better to treat only those who have progressed to stage IV (metastatic) cancer
if they want to be poisoned. And given
the small benefit of chemo, why prolong the illness with costly treatment that
lowers the quality of life? Yes, pharma
is very good at marketing
Hope’s Hypothesis (pharma’s
deceptive logic): that
chemo could make me a survivor. Chemotherapy in clinical trials doesn’t
have
a placebo group. It is given to terminal
patients, thus avoiding
long-term following with its side effects.
Remission is measured by imaging
observations of the tumors size.
Typically the tumor stops growing or shrinks for 3 months. Suppose the
average death occurs at 12 months
and that 20% die in 3 months; and 5% are live 2 years—the length of the trial.
That
does not prove that a few patients had an atypical positive response to the
drugs. Rather a few patients had indolent
metastatic cancer and would
have lived that long without the chemo.
In the 60s, prior to chemo some survived for years with metastatic
cancer. Today the patients receiving a
poisonous cocktail (typically 3 drugs) some will die from side effects such as
opportunist diseases for stage II and III, and many also for stage I, even when
the literature cautions against aggressive treatment. These patients believe
that the chemo will
destroy all the cancer missed by surgery, and the oncologist promotes this
belief. Moreover, the horrible side
effects will be downplayed. Instead
the oncologist sells Hope Hypothesis; pharma makes billions;
and the patients suffer. The evidence
basis always is biased in favor or pharma.
For an account of trial distortions read Bad Pharma by Dr. Ben Goldacre.
Pharma’s clinical trials are not about uncovering side effects or
indolent metastatic cancer, but about marketing. I certainly would fall for
Hope’s Hypothesis,
unless the cancer I had could be for some be cured based upon clear published
evidence. Remission isn’t a cure!
|
IF CHEMO CAN’T CURE
METASTATIC CANCER, THEN IT CAN’T CURE INDOLENT CANCER. They are essentially the same but for the
ability to fool the immune system. There is not an atypical positive response
for a subgroup; those terminal patients
have an indolent form of the cancer. The term “Survival” applied to chemo means “delays death”
a few months.
Like soldiers, doctors are believers, thus they sell their faith in
chemo.
|
Side effects: because chemotherapy consists of
chemicals that blocks essential processes, major side effects are the
norm. Among the effects, an assortment
of sickness symptom (nausea, pain, weakness, etc.) that is sufficient for about
half to modify or forgo full treatment.
There is a significant mortality risk because of suppression of the
production of red and white blood cells.
Typhlitis is an intestinal infection with a “very poor prognosis”.
Anemia and bleeding are blood suppression consequence along with
fatigue. Long-term consequences include
weakness and fatigue, an increased risk for new cancers, heart attack,
infertility, & damage to the heart, kidney, liver, intestines, hearing, brain, skin, and other organs. Chemo brain (PCCI) is a significant cognitive dysfunction; for
some “lasting 10 years or more” Wiki, A 1980 study of various cancers found, “…this was
surprising, due to the fact that a majority of the drugs administered in this
study are known to not cross the blood brain barrier (BBB)… Commonly describe
as affecting vision,
memory, coordination, attention, understanding…” Other studies have
added a psychiatric
dimension. In a 2013 summation of imaging studies both brain volume and neural activities
were down--both short and
long-term. Increased mortality is grossly
under reported, only cancer
deaths are counted, quality of life reduced and years lost.
JK’s Hope’s
Hypothesis--Positive Choices
In 1924 Otto Warburg one of the leading biochemists of the 20th
century and Nobel Laurette published his findings that cancers have abnormal
glucose metabolism and abnormal mitochondria.
Since as described above cancer is dependent essentially on glucose
fermentation, I would starve the cancer.
I would start with a water fast[9]
of 14 days or longer. At the end of the fast, I would go on a ketogenic diet
and even limit fiber.[10] Protein limited to 25-35
grams a day to
prevent loss of muscle mass. The amino
acid glutamine is another fuel for cancer, thus the low protein diet. With its
calories limited, for mot the growth
stops and the cancer shrinks. How
effective depends to a large extent on how crippled the mitochondria is, and if
some can still metabolize fat to some extent.
I would also become current on the latest work on diet. Currently work
is being done to limit
glutamine (another functional metabolic substrate), and supply cancer with a
optical isomer of glucose that it can’t metabolize. It would be a high
fat diet since cancer with
their defective mitochondria can’t metabolize fats. Hyperbolic oxygen
has also been shown to
promote the death of cancer cells. I would
also have the tumor removed as soon as possible. I would be less aggressive
in staving the
cancer if it was a local stage 1 cancer with a favorable biopsy report. Assuming
it is stage 2 or in a tissue that
has a high mortality rate, I would adhere strictly to the diet and go on
repeated fasts using fat for energy or try alternate day fasting. I would also
take 2 grams of aspirin
daily. Aspirin has
the highest
cure rate of all chemotherapies for stage
I, II, and III, and aspirin prevents cancer. (Oncologists hear a much different
account at
pharma’s continuing education classes.) Breast
cancer survival is up 66%
by stimulating necrosis
factor TNF; colon
cancer survival up 74%, & others for stages I, II & III; but does not increase
survival of metastatic cancer, yet should lengthen survival. Aspirin reduces
risk of
cancer evolving into a fatal cancer by its effect upon 3 bodily defenses: as a COX-2 inhibitor,
upon nitrous oxide (NO) system of
endothelial cells, and stimulation of the body’s system for destruction of
abnormal cells (apoptosis). Aspirin
increases survival of glandular, blood, & epithelial cancers. Also aspirin reduces
the risk for most cancers by promoting various necrosis factors and inhibition
of JNK which “regulates several important cellular functions including cell
growth, differentiation, survival and apoptosis” Wiki. Risk various tissues: reduction
of
“63% colon, 39% breast, 36% lung,
and 39% prostate cancer, also for esophageal 73%, stomach 62%, and ovarian
cancer 47%” also Hodgkin's
disease, and adult
leukemia, melanoma
55%. Other
studies have
shown that aspirin promotes
the death of abnormal cells through the natural mechanism of apoptosis by stimulating
tumor
necrosis factor NF-B,
by p38
& JNK. Long
term,
but low dose is insufficient because of drug
tolerance. Moreover the
increase risk of ulcer is in the US
Physician’s Study 1 per 1780
patient years with 325
bi-daily. At dose of 975 mg daily, the
ulcer risk is about 1 per 300 patient years.
In the Physician’s
Study the rate
of heart attack was reduced 44%. With higher dose of 325 mg daily, it
has an
inhibitory effect upon atherosclerosis that would be statistically significant
after 3 years-- and also its inhibitory effect upon cancer. The positive results
in journal articles are
based on general population studies. For
example a study
published in 1991 on cancer
prevention based on
lifestyle of 662,424 adults found that those who took 16 or more aspirin a
month had a 50% reduction in colon-cancer deaths (measured 1982-88). Similar
study using
nurses
found similar benefits for breast prevention
& survival. Pharma of course doesn’t fund clinical trials
for aspirin except to “demonstrate” its risk and ineffectiveness. The
positive information sits in journals,
while pharma friendly organizations using marketing studies produce treatment
guidelines on cancer and prevention of heart attacks which warn about the grave
risk of stomach bleeds that counters the modest benefits of low dose aspirin; a
message repeated in continuing education classes. I would also take testosterone
(and if a
woman estradiol with progesterone) since the sex hormones like other steroid
promote healing. One study found HRT
subsequent to breast cancer resulted in a substantial reduction in cancer
mortality. This is what I would do and
advise my wife to do.
Recommended
lectures
***** Targeting
Energy Metabolism in Brain Cancer 21
min, 113,000 views by Prof Thomas Seyfried, leading research to audience of
fellow scientists on how to starve cancer which depends on glucose metabolism and
thus cause its apoptosis through ketogenic diet. Cancer cells
have damaged mitochondria that metabolized glucose & glutamine-- read his Cancer
as a Metabolic Disease s. https://www.youtube.com/watch?v=sBjnWfT8HbQ&hd=1
Excellent
*****Cancer
as a Mitochondrial Metabolic Disease, 60
min, 13,000 views by Prof Thomas Seyfried, similar to the above, but with more
such as the role of macrophages, more on diet, glutamine, and how current
standard treatment kills their patients. https://www.youtube.com/watch?v=dm_ob5u9FdM
Excellent
*****
The Ketogenic Diet and Cancer
152,000 views, 30 minutes Dr. John Bregman radiologist recommends intermittent
fasting, with 8 hour window for eating and ketogenic diet misses glutamine,
critical of standard treatment. https://www.youtube.com/watch?v=Q9socQcwPIs
Excellent.
For more go to section 4 of this link Part 7 Videos
food, drugs, health YouTube
^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^end
[1] As
of now I don’t know enough about lymphomas and leukemias to predict the effects
of energy restriction.
[3]
“Only a small subset of tumor cells has the power to proliferate and expand…
share treats with stem cells…. Spring
forth from regulator failures in damaged stem cells… cancer treatments must
target cancer-stem cells” at
p, 42 As per above, not stem cells but TAM in which macrophage has turned on
certain oncogenic genes in the tumor.
[4]
Macrophages are large immune cells which function to clean up cell debris,
engulf foreign substance, microbes, cancer cells, stimulate immune system,
decrease immune reaction, encourage repair (M2 macrophage) signal for other
immune cells
[5]
Most stage I. II, & III cancers are cured by excision; commonly estimated
at 85% or more according to several journal articles.
[6] If
we dropped the few cancers that lives are saved (testicular, some leukemia-s
and lymphomas) the average would be 2 months.
[7] As
mentioned prior bias is the norm for pharma-funded studies. For example those
who die during the period
of chemo treatment are doped out of the study as too those who drop out because
of severe side effects, and their side effects are not included in the journal
article. Moreover, the post-marketing
studies (after a patent has been granted) are of the lowest quality. Read Ben
Goldacre’s Bad Pharm and Marcia
Angell How Drug Companies Deceive Us—and
on YouTube.
[8]
Stage I is local, stage II is invading adjacent tissue, and stage III is also
found in lymph nodes; stage IV is metastatic, found in other tissues such as
the liver, bone, brain, etc.
[9]
This would include tea with lemon juice and possible bone broth (See Fung,
Obesity Code P. 265)
[10]
As much as half the calories from fiber are made available through the
metabolism by intestinal bacteria.
Though it doesn’t raise insulin because of low quantity it supplies
glucose to the cancer.
CHEMO THAT CAN’T
CURE METASTATIC CANCER, THUS IT CAN’T CURE INDOLENT CANCER. They are essentially the same but
for the ability to fool the immune system. There is not an atypical positive
response for a subgroup; those terminal patients have an indolent form of the
cancer. The term “Survival” applied to chemo means “delays
death” a few months. Like soldiers, doctors are believers, thus
they sell their faith in chemo.
There
is a sales pitch for chemotherapy based upon bad logic. An example will make
it clear. The 2 year survival for untreated small cell
lung cancer average is 9 month, with 95 dying within 2 years. Chemo therapy
adds to the bell curve 2
months. Thus average survival is 11
months, and 95% die within 2 years 2 months.
Gertrude has small cell breast
cancer, and would untreated live average of 9 months. If she elects treatment,
she will be dead in
the 11th month. Treatment
doesn’t place Gertrude in the fortunate group of living over 2 years.
If,
for example a stage 3 breast cancer (65%
chance that it is metastatic) turns out to be metastatic the results is the
same with chemo, only now
that person lives 2 months longer. Chemo
doesn’t convert doesn’t change the course of events. Metastatic
cancer is like a time bomb, set to
kill its host after so many months. For
those who have an indolent non-metastatic cancer, the operation entails they
are a cancer survivor. If she is a
survivor without chemo, electing chemotherapy, she shortened her life by years. I
estimate at least 4.5 years. Millions of people undergo pointless chemo that
shortens their lives, and most of them falsely believe they are a survivor
because of the chemo.
Currently 3/14 there is a problem with the Google Chrome and the Internet Explorer browsers
of page width, but not with Mozilla.
CANCER basics &
CHEMOTHERAPY– 13 pgs -- 10/18/13
1)
While beyond the scope
of this paper, it is essential to understand the inroads made upon medical
science by corporate medicine. Corporate
medicine is market driven; medical science evidence driven. These
two approaches result in different
explanations concerning cancer. The goal here is to understand the general
basic biology of cancer and its treatment options based quality scientific
evidence—without market considerations. What follows is based upon sound
science with sources. Marketing science is
driven by profits, & thus promotes aggressive treatments. Pharma’s
marketing ploys confirms Harvard Prof. Dr. Marcia
Angell’s observation that we have “the worst system we
could imagine.” To learn more read Marketing
Science and its
links.
2)
The primary goal of this
explanation of the biology concerning cancer is to understand the benefits and
limitations of chemotherapy. This requires
an explanation of the biology of cancer, a topic I have long studied. Since
cancer involves a broad group of diseases, the exceptions to the generalities
are often excluded (the object is to understand what cancer is; thus not to
bury the reader in details). Cancer is a
line of body cells that have through mutations and often stem cells developed
the ability to spread rapidly. There are 7 essential types of mutations for turning
a cell into a cancerous cell line, and they involve over a hundred biochemical
cellular activities. Most chemotherapies
hinder one of these essential processes, and thus it must be applied short
term—only a few chemotherapies are curative (see paragraph 16). With corporate
medicine, this treatment of
cancer is sold as effective, but most aren’t.
Radiation and excision, by
removing an indolent cancer, reduces the risk of mutating into metastatic
cancer. If the tumor is in fact a
cancer and has already metastasized, the prognosis is very, very poor: excision,
radiation, and chemotherapy are
ineffective at preventing the fatal outcome.
Metastatic cancer can be indolent and take years to be diagnosed. Chemotherapy
does not destroy either the
indolent or aggressive cancers, though pharma and physicians will try to
persuade you otherwise. Chemotherapies
shut temporarily off an essential bodily
process, and thus effects also cancer cells.
Once therapy has been stopped, the essential process, such as making new
capillaries, resumes. Life extension
from chemotherapy in terminal patient averages 2 to 3 months. It is not a magic
bullet that destroys cancer
cells. It affect upon non-metastatic cancer is not
worth the side effects. Chemotherapy
won’t prevent an indolent cancer from at some future date becoming
metastatic. It is all a matter of
numbers, and clinical trials for FDA approval are on terminal cancer patients,
and are barely better than a placebo (no treatment). Once approved, they are
marketed using
tobacco science for all stages of cancer.
Pharma manipulation of the results,
is the norm because effective peer review is impossible. When administered in office, the oncologist
receives a spread between what is billed insurance and their bulk price for the
drugs, plus a fee for treatment. For the
reasons just stated early only excision and irradiating the cancer are effective. This
paper in it discussion of the biology
cancer reveals why chemotherapy fails to cure.
3) “A benign tumor is a mass of
cells (tumor) that lacks the ability to invade neighboring tissues or metastasize. These characteristics are required for a tumor to be defined as cancerous and therefore benign tumors are non-cancerous.
Also, benign tumors generally have
a slower growth rate than malignant tumors and the tumor cells are usually more
differentiated (cells have normal features). [1][2][3]
Benign tumors are typically surrounded
by an outer surface (fibrous sheath of connective tissue) or remain with the epithelium.[4]
Common examples
of benign tumors include moles (nevi), colon polyps, and uterine fibroids (leiomyomas). Although
benign tumors will not metastasize
or locally invade tissues, some types may still produce negative health
effects. The growth of benign tumors
produce a "mass
effect" that can
compress tissues and may cause nerve damage, reduction of blood to an area of
the body (ischaemia), tissue death (necrosis) and organ damage. The mass affect of tumors are more prominent
if the tumor is within an enclosed space such as the cranium, respiratory tract, sinus or inside bones. Tumors of endocrine tissues may overproduce certain hormones, especially when the cells are well
differentiated. Examples include thyroid adenomas
and adrenocortical
adenomas.[1] Although most
benign tumors are not life-threatening, many
types of benign tumors can become malignant through a process known as tumor
progression.[5] For this reason and
other possible negative health effects, some
benign tumors are removed by surgery.[6]” Wiki. Unfortunately pharma who profit
from overtreatment of benign tumors, promotes guidelines that are contrary to
the best interests of patients. This
practice has been exposed for the prostate, breast, thyroid, cervix, uterus
and ovaries, where studies
have shown that aggressive treatment causes more harm than good—and undoubted for
other tissues.
4) Cancer (malignant
neoplasm) is a broad
spectrum of diseases involving improperly regulated cell growth. For that cell
growth to become
life-threatening it must be capable of sufficient reproduction so as to disrupt
essential bodily processes. Over 80% of
fatal cancers spread to more distant part of the body through the lymphatic or
blood systems—some such as cerebral cancer often don’t. With the
exception of blood and lymphatic
cancers, they form hard tumors. “One of
the most
important factors in classifying a tumor as benign or malignant is its invasive
potential” Wiki. “If a tumor lacks the ability to invade
adjacent tissues or spread to distant sites by metastasizing
then it is benign, whereas invasive or
metastatic tumors are malignant.[1] For this reason, benign tumors are
not classed as
cancer”[2] Wiki. The degree of dysplasia (abnormal development of
tumor & it’s cells) does not make a tumor cancerous. To be cancer
it must be invasive. “Not all tumors are cancerous, benign
tumors do not invade neighboring tissues and do not metastasize” Wiki.
Unfortunately based on biopsy and microscopic examination of tissue and
corporate medicine, many of these benign tumors are called cancerous. The
removal of a few benign tumors can be
justified because of the high risk of becoming cancerous; however, in most
cases low-risk benign tumors are removed.
Often both are mislabeled “carcinoma”.
Guideline then require excision (or irradiation) and chemotherapy. A
number of quality studies have shown that this aggressive approach does more
harm than good. The 800 pound gorilla (pharma), using marketing science,
has
worked the treatment-guideline committees, and thus compel physicians to treat tumors
aggressively—compel though hospital administrators, and the risk of litigation
based on failure to follow guidelines.
5) “Cancer
cells are cells
that grow and divide at an unregulated,
quickened pace. Although cancer cells
can be quite common in a person they are only malignant when the other cells
(particularly natural killer cells, cytotoxic lymphocytes) fail to recognize
and/or destroy them.[1] The failure to recognize cancer cells
is caused by the lack of particular co-stimulated molecules that aid in the way antigens react with lymphocytes.[2] Other factors pay a role including viruses,
immune system issues, genetics, environmental pollutants including radiation
which promote random mutations of the DNA code, age, and too much of SP2
protein which may turn stem cells into cancer cells” Wiki. “Genetic and epigenetic
changes can occur at many levels, from gain or loss of entire chromosomes, to a
mutation affecting a single DNA nucleotide, or to silencing or
activating a microRNA that controls expression of 100 to 500 genes.[4][5]
6)
“Oncogenesis
(carcinogenesis): is literally the creation of cancer. It is a process by which normal cells are transformed into cancer cells.
It is characterized by a
progression of changes at the cellular genetic and epigenetic that ultimately reprogram a cell
to undergo uncontrolled cell division, thus forming a
malignant mass. Cell division is a physiological
process that occurs in almost all tissues and under many circumstances. Under
normal circumstances, the balance
between proliferation and programmed cell death, usually in the form of apoptosis, is maintained by
tightly regulating both processes to ensure the integrity of organs and
tissues. Only certain mutations and epimutations [genes that regulate the expression
of other genes] in DNA
that disrupt the orderly process can lead to cancer. These changes may remain
through cell divisions for the remainder of the cell's
life and may also last for
multiple generations. The majority of potential mutations and epimutations will
have no bearing on cancer” Wiki.
7) “A proto-oncogene is
a normal gene that can become an
oncogene due to mutations or increased expression. The resultant
protein may be termed an oncoprotein.[10] Proto-oncogenes
code for proteins that help to regulate cell growth and differentiation. Proto-oncogenes are often involved in signal transduction and execution of mitogenic signals,
usually
through their protein products. Upon activation,
a proto-oncogene (or its product) becomes a tumor-inducing agent, an oncogene.[11] The
proto-oncogene can become an oncogene by
a relatively small modification of its original function” Wiki.
|
 |
|
8) Stem cells
|
Stem
Cell
|
Progenitor
Cell
|
|
Self-renewal in vivo
|
Unlimited
|
Limited
|
|
Self-renewal in vitro
|
Unlimited
|
Limited
|
|
Potentiality
|
Multipotent
|
Unipotent, sometimes oligopotent
|
|
Maintenance of self-renewal
|
Yes
|
No
|
|
Population
|
Reaches maximum number of cells
before differentiating
|
Does not reach maximum
population
|
Stem cells are undifferentiated biological cells, that can differentiate into specialized cells
and can divide (through mitosis) to produce more stem
cells. In mammals, there are two broad types of stem cells: embryonic stem cells, which are isolated from the inner cell mass of blastocysts, and adult stem cells, which are found in
various tissues. In adult organisms,
stem cells
and progenitor cells act as a repair system for the body,
replenishing adult
tissues. Stem cells maintain the
normal turnover of regenerative organs, such as blood, skin, or intestinal
tissues. Stem cells possess two
properties: self renewal (to maintain
through cell division the
undifferentiated state) and potency
(to give rise to any mature cell type). For
example, the defining test for a
bone marrow or hematopoietic stem cell (HSC) is the ability to transplant
one cell and save an
individual without HSCs. In this case, a stem cell must be able to produce new
blood cells and immune cells over a long term, demonstrating potency. Stem cells can also be isolated by their
possession of a distinctive set of cell surface markers. Most adult stem
cells are
lineage-restricted (multipotent) and are generally referred to by their tissue origin (mesenchymal stem cell, adipose-derived stem cell, endothelial stem cell, dental pulp stem cell, etc.).[28][29] Induced
pluripotent, these are not adult stem cells, but rather adult cells (e.g.
epithelial cells) reprogrammed to
give rise to pluripotent capabilities. Using genetic reprogramming with protein transcription factors, pluripotent stem cells equivalent to embryonic stem cells have been derived from human adult
skin tissue.[53][54][55] Adult stem cells
(somatic stem cells)
9) A progenitor cell is a biological cell that,
like a stem cell, has a tendency to differentiate into a
specific type of cell, but is already more specific than a stem cell and is
pushed to differentiate into its "target" cell. The most important
difference between stem cells and progenitor cells is that stem cells can
replicate indefinitely, whereas progenitor cells can divide only a limited
number of times. The
majority of progenitor cells lie dormant or possess little activity in the tissue in
which they reside. They exhibit slow growth and
their main role is to replace cells lost by normal attrition. In case of tissue
injury, damaged or dead cells, progenitor cells can be activated. Growth factors or cytokines are
two substances that trigger the progenitors to mobilize toward the damaged
tissue. At the same time, they start to differentiate into the target cells. “Symmetric division
gives rise to two identical daughter cells both endowed with stem cell
properties. Asymmetric division, on the other hand, produces only one stem cell
and a progenitor cell with
limited self-renewal potential” Wiki.
10) A transcription-n factor (sometimes called a sequence-specific DNA-binding factor) is a protein that binds to specific DNA sequences, thereby controlling
the flow (or transcription) of genetic information from DNA to messenger RNA.[1][2] Transcription factors perform this function
alone or with other proteins in a complex, by promoting (as an activator), or blocking (as a repressor) the recruitment of RNA polymerase(the enzyme that
performs the transcription of genetic information
from DNA to RNA) to specific genes.[3][4][5] A defining feature of
transcription factors is that they contain one or more DNA-binding domains(DBDs), which attach to specific sequences of DNA
adjacent to the genes that they regulate.[6][7] Additional proteins such as coactivators, chromatin remodelers, histone acetylases, deacetylases, kinases, and methylases, while also playing
crucial roles in gene regulation, lack DNA-binding domains, and, therefore, are
not classified as transcription factors.[8] Many transcription factors are either tumor suppressors or oncogenes, and, thus, mutations
or aberrant regulation of them is associated with cancer. Three groups of
transcription factors are known to be important in human cancer: (1) the NF-kappaB andAP-1 families, (2) the STAT family and (3) the steroid receptors.[73]
11) “Cancerous
Stem Cells (CSCs): The role of stems cells is complex, varied,
only partially revealed, and very uncertain.
A number of factors support their role, but just what it is need
elucidation. A major problem consists of
identification; viz., differentiating between stoma cells turned cancerous and
that of stem cells turned cancerous. A
number of paths involving stem cells as the source of the malignant tumor, or
as the driving force behind progenitor cells, or functioning in the healing
process to stimulate the growth of benign tumors that emit an appropriate
signal for this process. Whatever way or
ways, CSC would explain the
variability of cell lines in cancerous tumors and their rapid growth. A third
issue clouding the research is that
that only a small percentage of CSCs
have the ability of generating a tumor.
“In human acute myeloid leukemia the frequency of these cells is
less than 1 in 10,000[9]. Many tumors are very heterogeneous and contain multiple cell types native to the host organ. Heterogeneity
is commonly retained
by tumor metastases. This implies that the cell that produced them had the
capacity to differentiate into multiple cell types. In other words, it possessed
multi-differentiative potential, a classical hallmark of stem cells[9] One important distinction that will often be
raised is that the cell of origin for a tumor cannot be demonstrated
using the cancer stem cell
as a model. This is because cancer stem cells are isolated from end-stage tumors. Therefore,
describing CSCs as a cell of origin
is often an inaccurate claim, even though a cancer stem cell is capable of
initiating new tumor formation. Tissues
with high rates of turnover, such as skin and colon are likely to involve CSCs,
since they are more active in
such tissues. Like normal stem cells, CSCs can have “the ability to form
anchorage-independent spheres.” Metastatic
cancer stem cells: Metastasis causes 80% of tumor lethality in
patients. Since cancerous tumors are
made up of different cells (see illustration above), not every tumor cell has
the ability to metastasize. This “potential depends on factors that determine
growth, angiogenesis
[growth of new blood vessels], invasion and other basic processes of tumor cells. Many tumors are very heterogeneous and contain multiple cell types native to the host organ. Heterogeneity
is commonly retained
by tumor metastases. This implies that the cell that produced them had the
capacity to generate multiple cell types. In other words, it possessed
multi-differentiative potential, a classic hallmark of stem cells[9]” Wiki. “To
date, researchers have reported findings evidence of cancerous stem cells in
tumors of breast, brain, skin, colon prostate, pancreas, and liver, among
others…. At least some cancers follow the stem cell model… Nor do researchers
understand how cancer stem cells originate;, how often they derive from normal
stem cells, or whether each tumor has just a few or many of the cells. Some
of the latest study results suggest that
a complex mix of both the standard model [one cell line] and the cancer stem
cell idea comes closest to elucidating how cancers form.” Cassandra Willyard,
Scientific American Aug,
2011, p. 34)
12) Mechanisms
for preventing a cell line from becoming malignant:
Cancer
is the result of a series of mutations that confer on one cell line (from
a single cell) a number of properties for which various biological constraints
on proliferation have been modified. In
most cases the cell line continues to mutate rapidly and presents when examined
presents significant variation in physical form, function, and mutations. Nevertheless,
the tissue from which the
cancerous cell line is derived very significant effects prognosis. Oncogenesis
involves typically 7 basic
families of changes (leukemia 4) which are governed by many genes. Typical of
most cancer cell lines is an
oncogene failing to limit the rate of mutations thus causing an abnormally high
rate of mutations. This increases the
probability of a lethal cancer. Thus in
addition to transformation into oncogenes, there are many other noncancerous
mutations which affect the cancerous cell line.
Thus most tumors under the microscope show a high degree of abnormal
cells (see illustration above). A second
key to malignancy is the involvement of stem cells. A few stems cells are found
in benign tumors,
in metastatic, and in invasive cancers.
Their important roles have been an object of intensive research for over
3 decades (see section below). While the
tumor is small, most ultimately fatal cancers develop the ability to
metastasize. Nevertheless, an indolent
invasive cancer as it ages can evolving into a fatal cancer. Early detection
has been oversold (a topic
developed below with breast cancer used as an example), and the removal benign
potentially cancerous tumors has for most tissues minimal effect upon
lethality. Such benign tumors are too
often called stage I cancers. Under 10%
of all cancers involve an inherited genetic mutation disabling a gene which
promotes the accurate reproduction of the DNA during mitosis, and thereby
accelerating the rate of ocogenetic mutation and subsequent cancer. Those with
the inherited defect have a
cellular
mutation
rate of around 10 fold that of the
norm. Another common way the rate of
mutation accelerates is through the exposure of tissues to radiation or
chemicals which
promote mutations. Tobacco smoke
contains such chemicals, and increases the risk of cancer in most tissues; for
example pancreatic cancer 250%. Counting
environment including infectious causes, they account for about 50% of all
cancers; the rest are a matter of chance including the 10% inherited oncogenes. There
are 15 general types of functional
alterations that contribute to turning a single cell line into a life-threatening
cancer; however, not all 15 types of are essential.
The blastocyst is a structure formed in the
early gestation of vertebrates. It is preceded
by the morula. It possesses an inner cell mass (ICM), or embryoblast, which
subsequently
forms the embryo, and an outer layer of cells, or trophoblast, surrounding the inner cell mass and a
fluid-filled cavity known as the blastocoele. The human blastocyst comprises 70-100 cells.
Cell potency is a general term which describes a stem cell's ability
to differentiate into different cell
types.[1] [2] The
more cell
types a stem cell can differentiate into, the greater its potency. Potency
is also described as the gene activation potential within a cell which like a
continuum begins with totipotency to designate a cell with the
most differentiation potential, pluripotency, multipotency, oligopotency and finally unipotency.
13) Changes:
1. Rapid cell division by turning on the
chemical signals for mitosis and leaving it on.
VERY COMMON
2.
Angiogenesis: Stimulating the formation of new capillaries to assure
adequate oxygen supply for continued growth of the abnormal cells. ESSENTIAL
but for leukemia
3.
Limitless
replication of
one cell line by
turning on telomerase, which adds telomeres to make the cell line immortal. Cell divisions in normal cells are limited to
about 50 replications. ESSENTIAL
4.
Mutations affecting adhesiveness, to
free the cells from the matrix which holds them in
place. VERY COMMON
5.
Invade
adjacent tissues: Organs are
enveloped in a membrane (muscle, intestine, lung, etc). Most cancers fairly
early develop the ability
to grow through the membrane and invade adjacent tissues. VERY COMMON
6.
Metastasize:
have microscopic colonies of the tumor
relocate in other sites. This involves
mutations affecting the ability to enter capillaries, which thus permits single
cells to migrate. ESSENTIAL for the 80%
that are metastatic cancers.
7.
Fool immune system for migration to distant tissues: change markers
on the cell wall so cells do not appear as
foreign to the immune system, which will destroy those cells. Which tissues
a cancer migrates to is highly
dependent upon the markers. ESSENTIAL
for metastatic cancer.
8.
Being able to both enter and leave blood vessels like the
way lymphocytes do by secreting a factor which
allows them to enter a capillary and then at another site to pass out of the
capillary again--a class of compounds known as SRC kinase. ESSENTIAL for metastatic
cancer.
9.
Infection including oncovirus can
increase risk of cancer. The WHO estimates that
18% (1/6th) of cancers have as a causal
vector an infection, of which two thirds are viral.
10.
Some cancers have abnormal DNA due to gross
changes in the chromosome that consist of translocation, duplication, deletion,
or inversion. This type of abnormality
results in the imperfect expression of genes on that chromosome. MODERATELY
COMMON
11.
Environment causes,
exposure to carcinogens and ionizing radiation by causing mutation—for a large
population, a causal factor in about 30% of cancer.
12.
Disabling of the gene that check the accuracy of replication
of DNA during mitosis, such as
p53, BRAC1, BRAC2, etc. Given the number of mutations required for cancer, most
cancerous cell lines have this system disable to some extent. Not all mutations
disable the checking
process, thus the risk factor depends on the mutation. When a specific cancer runs in a family, the
cause could be an inherited mutation. Of one of these genes. COMMON
13.
Programmed
cell death (apoptosis)
is disabled. Cancers are immortal: not
limited to about 50 cell division. ESSENTIAL
14.
Heterogeneity
results from the high rate of mutation in most cancers, “tumor population
exhibit functional, and tumors are formed from cells with various proliferative
and differentiate capacities” Wiki, and. VERY COMMON
15. Excrete
growth factors which
enable
the cancer to attract stem cells which then help support the growth of the
tumor by stimulating the growth of capillaries and other structures needed to
support a large tumor. ESSENTIAL
16. Natural
selection favors
the uncontrolled
reproduction of the cancerous cell line.
17. Pluripotent cells created by action of
stem cells create from stoma cells. COMMON
This is a list of the key
types of mutations On average, for example, “15 driver mutations" and 60
"passenger" mutations are found in colon cancers.[2] Mutations in those certain types
of genes that play vital
roles in cell division, apoptosis (cell death), and mutations and epimutations
(see article Genome instability) in DNA repair genes
will cause a cell to lose control of its cell proliferation. This mass alternation
of genetic code in
malignant tissue is essential to the understanding of why cancer can develop
resistance to chemotherapy, and why invasive cancer given a couple of years has
a guestimate 20% chance of becoming metastatic.
Natural selection favors the cell line which can resist chemotherapy and
spread to distant organs. This raises the question against the backdrop of
orderly low rate of mutation stoma cells and
while others form tumors that are quite indolent; why is there a modest
percentage that are mutating at very high rates? How is this possible? One answer is mutations in genes which
promote accurate replication of DNA.
Another is the involvement of stem cells. Stems cells have the
ability to convert
stoma cells into progenitor cells as a way to promote re-growth are undifferentiated cells, found throughout the body after development,
that multiply by cell division to replenish dying cells and regenerate
damaged tissues.
14. Complexity—some examples
Chemical stimulation of angiogenesis is
performed by various angiogenic proteins, including several growth
factors.
This table is illustrative
of the number of orchestrated genes that are involved the production of new
blood vessels. Thus an epigenetic switch
is responsible for angiogenesis. That
for most tumors this switch is off, then at some point turned is evidence for
the role of stem cells.
In most cervical cancer, for example, a mutation causes the cell-to-cell
adhesive molecule E-carherin to be digested, and as a consequence the cancerous
cervical cell line can spread to distant tissues.
17) WHY
MOST CHEMOTHERAPIES DO NOT AFFECT THE LETHALITY
OF METASTATIC CANCER: The
fundamental problem is how to poison
or make dormant long-term, bodily cells that are malignant without also
poisoning or making dormant normal bodily cells. The difficulty arises because
cancerous cells
are nearly identical to normal cells.
There are a few very effective chemical therapies; most often in a
tissue for which major damage is not life threaten, such as testicles. A unique
marker on the cell wall or a unique
chemical process in that cell line can permit the development of a chemotherapy
that will destroy the metastatic distant tumors without destroying the adjacent
tissue. For the other types of tissue
where this is unlikely, pharma relies upon chemicals that are disrupting
cell division (reproduction). Most
cancers divide rapidly. “Thus
chemotherapy also harms normal cells
that divide rapidly in the bone marrow, digestive tract, and hair follicles, and to a lesser
extent slow dividing cells. This results in the
most common side-effects
of chemotherapy: myelo-suppression (decreased production of blood cells,
hence also immuno-suppression), mucositis
(inflammation of the
lining of the digestive tract), and alopecia (hair loss). Virtually
all chemotherapeutic regimens can cause depression of the immune system, often by paralysing
the bone marrow and leading
to a
decrease of white blood cells, red blood cells, and platelets” Wiki.
Indolent cancers
tend to respond much more
modestly to chemotherapy. Causing
damage and shut-down are why most chemotherapies are given short term. Thus
for aggressive cancers, the chemotherapy
does not eliminate the cancer, but rather produces a short remission and thus
prolongs life on average a few months.
18) PROBLEMS WITH
RESEARCH, JOURNAL PUBLICATIONS,
and AND GUIDELINES: Drug
companies push that everyone with cancer should be on chemotherapy at the
greatest dose for the longest time, and they do the research to “prove” it (see
Marketing Science and Side Effects). Given
that positive bias is the norm (average 32%),
and guidelines heavily rely upon junk science, a starting point would be to
look for published clinical trials show major advantages to the treated cohort,
and remember that side effects are always under-reported, and long-term ones
don‘t become statistically significant during the period of most studies and
often are not within the study’s protocol. The standard testing for
FDA patent of exclusivity is on terminal metastatic cancer patients, compared
to a placebo generally after the standard chemotherapy’s temporary remission
has ended and further chemotherapy is contra-indicated. If there is an average
life extension of a
couple of months for the treated cohort, the FDA grants a patent of
exclusivity. And though the FDA receives
the raw data during the approval process, they do not make it public, nor do
they review for accuracy the journal articles published based these
submissions. The 32% bias referred to
above was found in a study comparing the raw data submitted to the FDA compared
to its journal publication (raw data obtained through the Freedom of
Information Act). Such short-term
testing in terminal patients does not reveal most side effects. Unfortunately
the treatment is not tested on
those mostly likely to receive it, Stage I-III cancers. But should they, and
how to decide? Remember the marketing
department of pharma is involved in all aspects of their clinical trials and
they own the results. Given this, major
benefits must be demonstrated, as it is for the treatment of non-Hodgkin’s
lymphoma. Bias, junk science, junk
guidelines, and junk continuing education of doctors are the norm.
18) SHOULD
CHEMOTHERAPY BE GIVEN TO A STAGE I, II, OR III CANCER? Except for the most
lethal cancers, all too
often the chemotherapy is life shortening, because of its side effects upon
those who were cured through invasive treatment. Aggressive treatment of stages
I & II
shorten life, for breast cancer an average of 2.5—and this is not taught
oncologists in continuing education classes.
The journal article that documented this has been lost in the sea of
time and pharma sponsored articles.
Besides most doctors follow treatment
guidelines even when skeptical of its application.
Following radiation or
surgery, how beneficial is adjunct chemotherapy, maintenance (long-term)
chemotherapy, and neo-adjunct (prior to radiation/surgery)? A combination
of factors is germane: 1) the life expectancy of the patient following
excision of the cancer. 2) The health
consequences of the chemotherapy both on quality of life and duration. 3) The
cost of the chemotherapy and the
recommended subsequent drugs. 4) The effectiveness of the chemotherapy upon the
indolent excised cancer with in vitro chemo-sensitivity
testing. 5) The effectiveness of the chemotherapy upon
the malignant tissue found in adjacent lymph nodes. 6) The result of study of a matching or
placebo controlled study on the value of adjunct chemotherapy for stage I, II,
III cancers. Most studies are not
placebo control, so duration of cancer growth suppression (termed “remission”)
is the best substitute information.
Typically it averages the duration of the chemotherapy. Since the manufacturer
most likely funded the
study the results are biased over 30%, thus increased survival needs to be adjusted. An informed choice is not easy, made more difficult
by the system of corporate medicine and the vest interest the oncologist has in
aggressive treatment. Serving the patient’s best interest is lost
in the corporate system. Thus for
example chemotherapy as an adjunct treatment is pushed on patients without in
vitro testing of the drugs. There are
more profits in treating everyone. Moreover,
the costs of treatment upon the healthcare system and the need for a better
allocation of resources, this is not figured into the short-term maximization
of corporate profits.
19)
Three special cases for chemotherapy:
1) Salvage chemotherapy or palliative
chemotherapy is given without
curative intent, but simply to decrease tumor load and increase life
expectancy. For these regimens, a better toxicity profile is generally expected.
2) Curative
chemotherapy, such as for non-Hodgkin’s lymphoma and testicular cancer.
3) Some
newer anticancer drugs (for example, various monoclonal antibodies)
are not indiscriminately cytotoxic, but rather target proteins that are
abnormally expressed in cancer cells and that are essential for their growth. Such
treatments are often referred to as targeted therapy (as
distinct from classic chemotherapy). Their
lower immediate and obvious side
effects, doesn’t entail that there aren’t major long-term ones. And
being able to target the cancer does ipso
facto make them curative. Their use with
traditional chemotherapy should be carefully evaluated to remove business
bias.
20) Deciding
what to do
Read Marketing
Science then start
with the journal literature, oncology textbooks, http://www.wikipedia.org/, https://www.worstpills.org/, http://www.rxlist.com,
http://www.mayoclinic.com/, http://www.cochrane.org/, and the
http://www.merckmanuals.com/.
Be skeptical of the advice given by the oncologist. If you can’t
find strong evidence of major advantage
in all the articles for the chemotherapy than forgo such treatment. Write out
key point which promotes rational
analysis rather than a decision by a gut feeling, for which social
considerations play a major role.
Treatment choices ought to be solely based on the evidence.
For the few
patients who research the issues. Learn
to recognize the 1) unmerited positive enthusiasm in journal articles.
Bias is often found in the
conclusion and abstract sections that does not follow from the results of the
study. Convert results to the number of
patients that must be treated for 1 patient to show major life extension, Calculate
the average life extension of treated group.
One common fallacy is to conclude that a 2) subgroup will benefit atypically
from the chemotherapy and be
cured or have a prolonged remission.
This is the result of a statistical fallacy: by simple chance a few small
groups will do
better than the average (and a few will do worse). Without clear proof, don’t
assume that
slowing down the rate of mitosis (cell division) for a few months will produce
a cure for a subgroup of patients.
Look for 3) obvious issues that
should be measured but aren’t; all too often they aren’t because the
results aren’t in the interest of pharma. Most studies don’t follow long-term patients
or list all causes of death because pharma doesn’t like those results. It
is very convenient that they use terminal
patients, since side effects are very poorly reported and long-term ones don’t
occur. 4) Pharma actively downplays and
hides side effects. After FDA approval
for which pharma must
submit the raw data, the subsequent marketing studies are of a significant
lower standard since there is no review of the raw data. Many of these studies
are on non-metastatic
cancer. Don’t assume that there is an
honest evaluation of side effects. Most
studies do not have a placebo group, which make evaluation of net benefit
impossible.
Remember only those who
are pharma “friendly” receive funds for research, and pharma’s marketing
department is actively involved in all aspects of the project, and they often
ghost write the journal articles. 5)
Don’t assume that there isn’t substantial favorable bias for
the reported benefits of
chemotherapy. There are many ways to
create positive bias. Remember that this
is the way business is done.
Especially,
search for articles by critics
published in a major medical journal. These
articles often review the literature and perform a meta-study on the published
clinical trials that meet a higher standard.
But they can’t rise above pharma’s hold upon research, favorable bias is
the norm. Sometimes an article will glean
out of pharma funded studies the negative results. These critical articles meet
a higher standard that marketing studies to be published in a major journal. Also
in general older wisdom is not false, especially when it stands in the way of
profits for pharma. For example in our
article of natural estrogen there is listed 8 articles with links showing that
estrogen lowers the risk of metastatic
breast cancer deaths, the incidents of breast cancer, and the relapse. Also shown is that using certain progestins
in HRT the opposite consequences—with 4 links to journal articles. The
800 pound gorilla has rewritten the book
on HRT and breast cancer. Question
treatment guidelines, they are all pharma friendly. Remember
“The
pharmaceutical industry is the most lucrative, the most cynical and the least
ethical of all the industries. It is
like an octopus with tentacles that has infiltrated all the decision-making
bodies: world health organizations,
government agencies, parliaments, high administrations in health and hospitals
and the medical profession." Dr. Evan with Debre authors
of Guide Des 4,000
Medicaments Sept. 2012. There they list half the drugs that are
useless and dangerous. Population studies show that cancer, if it is
metastatic, chemotherapy and regular checkups make minor differences,
not enough to justify chemotherapy or frequent follow-up examinations.
21)
Atypical
cures, Hope’s hypothesis:
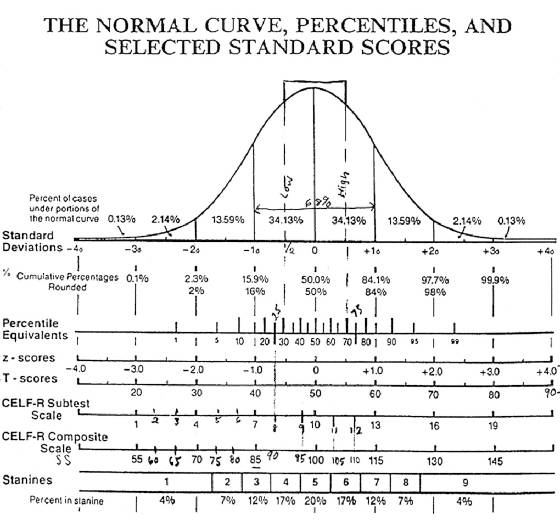
^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^ Non-technical summation
Cancer is
distinguished from a benign tumor by its ability to invade neighboring tissue
and sometimes spread to distant tissues (metastasize). Also benign tumors generally
have a slower
growth rate and are more differentiated (more normal cell features). This is
the first area where business has
blurred the distinction between benign and malignant and thus aggressively
treats with surgery and chemotherapy benign tumors, by calling them “carcinoma”.
Critics have pointed out the negative
consequences from such treatment of benig tumors of the breast prostate, and
thyroid cancers, and others by the adjunct chemotherapy following
excision. Benign breast tumors, called
“cancer”, when treated shorten life over 2.6 years. Another line
crossed is to treat a stage I &
II cancers aggressively where the risk for it being metastatic cancer is low
and the chemotherapy offers minor benefit.
With a few exceptions, chemotherapy doesn’t cure cancer, but rather
shuts down an essential biological process that affects the rate of cell
reproduction, including the cancers’.
This toxicity entails a limit to the chemotherapy. The average remission
for such treatments is
3 months. Both in the treated and
untreated groups there will be people who last years past the average (they
have indolent cancers); therefore consider only the average life extension.
Three special cases for chemotherapy:
1) Salvage chemotherapy or palliative
chemotherapy is given without
curative intent, but simply to decrease tumor load and increase life
expectancy. For these regimens, a better toxicity profile is generally
expected.
2) Curative
chemotherapy, such as for non-Hodgkin’s lymphoma and testicular cancer. Only
a few cell lines of metastatic cancers
can be cured. By chemotherapy.
3) Some
newer anticancer drugs (for example, various monoclonal antibodies)
are not indiscriminately cytotoxic, but rather target proteins that are
abnormally expressed in cancer cells and that are essential for their
growth. Such treatments are often
referred to as targeted therapy (as
distinct from classic chemotherapy).
But being able to target the cancer doesn’t make them curative.
The choice
of chemo and target therapy should be
carefully evaluated to remove business bias and the oncologist sales
pitch. Oncologists make the spread
between what they bill and the discount price.
Remember that excision produces over 95% of the cures for the common
types of cancer.
|
 |
|
|
 |
|
|
|