|
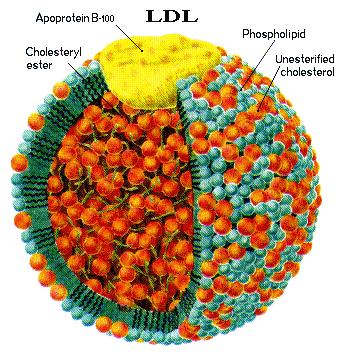
| phospholipids the major component of cell membrane |
|
| cholesterol esters, cholesterol bonded to a fat |
Short version (detailed technical version below) This article will be updated shortly to include the work of the
last 2 years on diet, metabolic syndrome, pathogens, LDL immune function, etc.
For confirmation from journal articles on primary role
of
infective agent enter into http://scholar.google.com/
terms such as bacteria + atherosclerosis. Journal
articles on LDL’s immune functions http://healthfully.org/rl/id8.html,
http://healthfully.org/rja/id1.html, and http://healthfully.org/rja/id1.html
and review article on infections causing
pathogenesis resulting in atherosclerosis by Uffre Ravnskov and Kilmer McCully
at http://healthfully.org/rl/id8.html. Also published are articles
on the Cholesterol Myth and Cholesterol
Myth, Source History.and list of best on YouTube
ATHEROSLEROSIS
AND HEART ATTACKS: the actual causes and how to
lower risks
Hardening
of the arteries also
called atherosclerosis (AS) causes cardiovascular disease (CVD). The leading
risk factor is infectious agents living within
the muscular wall of the arteries. These pathogens within the wall produce
toxins, which elicit a cleanup process that involves both LDL and HDL in that
they attach to these lipoproteins. HDL
& LDL besides transporting cholesterol and triglycerides have an immune
function. White blood cells enter the
inflammation zone as part of the system for controlling pathogens and their
toxins. It is acknowledged beyond
dispute that AS is an inflammatory condition.
The role of pathogens has
been demonstrated in hundreds of experiments that are published in journal
articles (http://scholar.google.com/),
yet the research articles are essentially ignored by a pharma which functions
to maximize its profits by lowering cholesterol and LDL with drugs. Prevent
in this case violates their fiduciary
obligation. The chorus of critics is
ignored by pharma who controls the education of doctors. Doctors are taught that pharma’s drugs are safe and effective. Blocking the production of LDL and
cholesterol not only doesn’t affect the inflammatory process, but has numerous
side effects, especially muscle pain and cognitive decline. Most affected are
senior, which constitute
2/3rds of the market. Numerous books and
documentaries are on the Cholesterol
Myth. Several factors accelerate this
process especially
chronic infection, diabetes, insulin resistance, and reactive chemicals such as
those from smoking cigarettes (carbon monoxide). Diabetes is associated with
a high level of
blood sugar, and sugar is a reactive chemical; also the high level of insulin
is associated with other health issues including obesity by promoting the
storage of fat, increased appetite and lowering metabolism that causes weight
gain. Hypertension in the vast
majority of cases is not
a cause of acute adverse events, but rather an indicator of AS, because
clogged-stiff arteries causes the heart to pump harder to adequately supply blood
to the organs. Because of the role of
pathogens and that 85% of heart attacks (MIs)
occur from the leaking of young immature plaque, just over half of all MIs
occurs to those in in the low risk group (normal blood pressure, non-smokers,
normal blood sugar, and normal LDL level).
Thus everyone is at
risk. Note: those with risk factors
such as hypertension (a
sign of AS) and diabetes are likely
to be currently producing much more young unstable plaque than those without
risk factors. Secondly the treating of
mature stable plaque with angioplasty and bypass operation is not in the
patient’s best interest. High level of
LDL and triglycerides is not a risk factor—part of the Cholesterol Myth. A second myth, started in the late 70s by our
government and shortly thereafter by governments around the world, holds that high
consumption of fats, especially saturated fats, and cholesterol are the primary
dietary cause for the rise in heart attacks and strokes between 1920 and 1970
(they ignored that 46%
of the people then smoked and long-term smoking over doubles the risk of heart
attacks). A low-fat diet entails eating
more carbs including sugars—which is great for the manufactured-food industry
and pharma. The critics of this dietary change
were ignored, and as a result we have the obesity and diabetes epidemics. To
reduce the risk of MI, follow a healthful life-style.
Start with a low carbohydrate-sugar
diet and exercise as the first line of defense. Saturated fats and monounsaturated fats
are the best sources to replace the energy from carbs. CoQ10 (Q10), which
is found in every cell in the body, should
be taken daily starting in
the teen years; it is the best of the fat soluble antioxidants. In addition
women starting with menopause and
continuing thereafter should take the natural HRT (estradiol
and progesterone), and men starting between 60 and 70 should take
testosterone. There is 50% reduction in
MI with estradiol; it lack is why cardiovascular disease and heart attacks
occur following menopause. Men on Testosterone are will exercise more, less
likely to develop metabolic syndrome (diabetes, hypertension, obesity, and AS),
and are more likely to survive an
MI. Both hormones have numerous other
healthful benefits such as the prevention of osteoporosis. For these reasons
KOLs instruct doctors against the use of hormones. Aspirin in the anti-inflammatory dose of 325 mg with meals
prevents atherogenesis, cancer, Alzheimer’s disease, and numerous other conditions. Thus pharma runs
junk clinical trials and then educates doctors to warn patients of the risk of
ulcers, though the risk increase is minor.
The perverse outcome is because all the other NSAIDs recommended by
physicians increase the risk of heart attacks—significantly enough for the American
Heart Association to issue a clear warning. I’d rather double the risk of an ulcer, than
not
lower the risk of the much more common heart attack by 50% and cancer by over
30%. Aspirin, estradiol, and Q10 along with
healthful lifestyle and low carb-sugar diet can stop the formation of new plaque, and thus over the next
4 years will greatly reduce the risk for heart attack and stroke as the body stops
making young unstable plaque, the cause of over 85% of heart attacks.
Note: and it gets worse,
read the section on Reyes syndrome
used to dissuade parents from giving children aspirin, and the article on acetaminophen for its health issue. We have a system of medical care based on the
advice of pharma’s KOLs and their treatment guidelines.
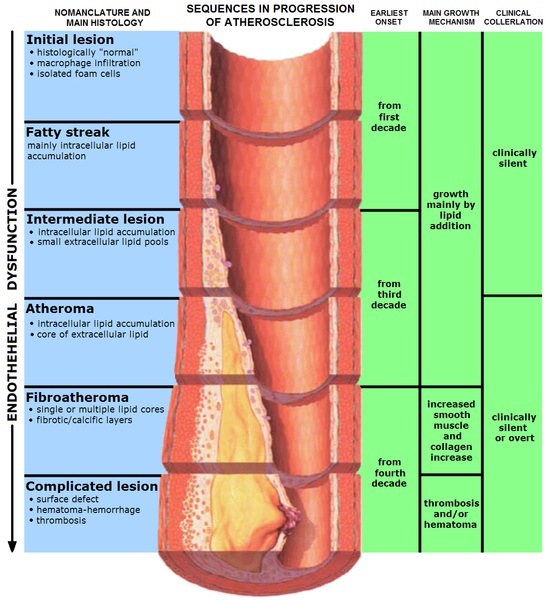
| Notice the wider diameter as plaque accumulates |
|
ATHEROGENESIS & Myocardial
Infarction -- 9 pgs., 11/23/14 (http://healthfully.org/rc/id12.html)
Coronary
artery disease (atherosclerotic heart disease) consists of plaque
formation in the tunica media
(muscular section) of the coronary arteries.
Plaque leaking from the artery wall is responsible for about 85% of all
myocardial infarctions (MI, heart
attacks). Pathogens play an initiating role in most if
not all cases leading to the development of atherogenic plaque (atheroma). Toxins and other reactive
chemical generated
by the pathogens attach to LDL and HDL in their immune system function.
Pharma acknowledges the inflammatory process,
but ascribes oxidative damage to LDL from other sources as the primary cause,
and ignores the immune function of LDL and HDL.
What follows is the pharma’s analysis of the process, then followed
ignored but well supported role of pathogens.
Pharma’s version: “Coronary
artery disease is the most common
type
of heart disease and cause of heart attacks. The
disease is caused by plaque building up along the inner walls of
the arteries of the heart [tunica media],
which narrows the arteries and restricts blood flow to the heart. It is the
leading cause of death worldwide. After
decades of progression, some of these atheromatous plaques may
rupture and (along with the activation of the blood clotting system) start limiting blood flow to the heart muscle. The disease is the most common cause of sudden death, and
the leading cause of death over the age of 20 years. Most commonly, unstable
young plaque ruptures
and may lead to an acute myocardial infarction (AMI)” Wiki. About 85% of AMI starts
with the leakage of unstable plaque that is sealed with a blood clot.
So what starts the process and what does the
plaque consist of, according to pharma’s key opinion leaders (KOLs)?
Plaque and
Atherogenesis:
A summation of process for developing cardiovascular
disease (CVD) from a 2009 Journal
article by a KOL: “Atherosclerosis
(AS) is now recognised as a chronic
inflammatory disease
occurring within the artery wall and ultimately responsible for myocardial
infarction, stroke and peripheral vascular disease. A
crucial step in atherogenesis is the infiltration of monocytes[1] into the sub-endothelial
space of large arteries where they
differentiate into macrophages and become functionally active. Macrophage[2] accumulation within plaques is a hallmark
of all stages of AS. Indeed, recent
studies have shown their presence has the potential to act as a non-invasive
marker of disease activity and plaque stability. Activated macrophages are major players in all
stages of lesion development. They not only accumulate lipids but also express
effector molecules that are pro-inflammatory, cytotoxic and chemotactic {KOL means macrophages absorb fats,[3] and
molecules that cause inflammation, tissue damage, and microorganism]. Furthermore, they secrete enzymes that degrade
extracellular matrix leading to plaque
destabilisation and increased risk of rupture. However, macrophages are
heterogeneous and when appropriately activated they have the potential to drive
tissue remodeling and ultimately vascular repair. Pharmacological modulation of macrophage
activities therefore represents an important strategy for the prevention and
treatment of AS and other
inflammatory diseases.” “ When the macrophages
engulf a large amount of the oxidized
cholesterol (as part of the disposal process) they are called foam cells because of appearance. In sufficient numbers they form the
fatty streaks of the plaques of atheroma in the innermost layer of the artery
wall. A protective fibrous cap normally
forms between the fatty deposits and the artery lining (the intima). These capped fatty
deposits (now called 'atheromas') produce enzymes that cause the artery to
enlarge over time. Atheromas within the vessel wall are soft and fragile with
little elasticity. Arteries constantly expand and contract with each heartbeat,
i.e., the pulse. In addition, the calcification
deposits between the outer portion of the atheroma and the muscular wall, as
they progress, lead
to a loss of elasticity
and stiffening of the artery as a whole” Wiki. “Hard, clogged
arteries are the principle cause of high blood pressure, but not MI.
Macrophages in their cleanup healing role for
young plaque secrete cytokines and protease that weaken the fibrous cap,
causing it to erode or rupture. The
newly
exposed sub-endothelium and pro-coagulant factor precipitate platelet
aggregation and local thrombus formation, sometimes leading to infarction [MI
& strokes]” AHA, 2013.
Atheroma: is an accumulation of degenerative
material in
the tunica intima (inner
muscular layer) of artery walls.
The material consists of (mostly) macrophage cells, or debris, containing lipids (cholesterol and
fatty acids), calcium and a variable amount
of fibrous connective tissue. The accumulated material forms a swelling in
the artery wall, which may intrude into the channel of the artery, narrowing it
and restricting blood flow. Atheroma occurs
in AS, which is one of the three subtypes of arteriosclerosis.
While
the early stages, based on gross appearance, have traditionally been termed fatty streaks by
pathologists, they are not composed of fat cells, i.e. adipose cells, but of accumulations
of white blood cells, especially macrophages, that have taken up oxidized LDL. After they accumulate large amounts of
cytoplasmic membranes (with associated high cholesterol content) they are
called foam cells. When foam cells die,[4]
their contents are released, which attracts more macrophages and creates an
extracellular lipid core near the center to inner surface of each
atherosclerotic plaque. Conversely, the outer, older portions of the plaque
become more calcified, less metabolically active and more physically stiff over
time. The older methods for understanding atheroma, dating to before World War
II, relied on autopsy data. Autopsy data has long shown initiation of fatty streaks in
later childhood with slow asymptomatic
progression over decades” Wiki. Stiff and constricted arteries are the cause of
hypertension. Younger plaque can leak
and cause a blockage downstream, which is further restricted by a blood
clot. This process causes the majority of
acute ischemic events (major heart attacks and strokes). This thrombosis process
can also affect other
organs such as the kidneys. “Older plaque is stable and unlikely to cause a
medical emergency, though, for example, it can cause stable angina. Most
MIs occur with less than 50% and typically
at locations with about 20% stenosis
(narrowing), prior to sudden lumen closure resulting in an MI” Wiki. Bypass operation
and angioplasty are done on vessels with typically a 70% or greater occlusion;
thus they do not reduce the risk of MI & death, but only manage angina pain. They
aren’t worth the side effects, including
pump head. “Atheroma and
changes in the artery wall usually result in small aneurysms (enlargements)
just large enough to compensate
for the extra wall thickness with no change in the lumen diameter. However,
eventually, typically as a result of rupture of (unstable) vulnerable plaques and
clots within the lumen over the plaque, stenosis (narrowing) of the vessel develops in some
areas. Less frequently, the artery enlarges so much that a gross aneurysmal enlargement
of the artery results. All three
results are often observed, at different locations, within the same
individual. Over time, atheromata
usually progress in size and thickness and induce the surrounding muscular
central region (the media) of the artery to
stretch out, termed remodeling, typically
just enough to compensate for their size such that the caliber of
the artery opening (lumen) remains unchanged
until typically over 50% of the artery wall cross-sectional area consists of
atheromatous tissue. If a rupture occurs
of the endothelium and fibrous cap, then a platelet and clotting response over
the rupture rapidly develops. Additionally, the rupture may result in a shower
of debris. Platelet and clot accumulation
over the rupture may produce
narrowing/closure of the lumen, and tissue damage may occur due to either
closure of the lumen resulting in loss of blood flow beyond the ruptured
atheroma and/or by occlusion of smaller downstream vessels by debris. This is the principal mechanism of myocardial infarction, stroke or
other related cardiovascular disease problems
including hypertension“ Wiki. So
what is causing the oxidation of LDL & driving the production of plaque?
[1] “Monocytes are a type of white blood
cell. They
are the largest of all leucocytes. They
are part of the innate immune system of vertebrates
including
all mammals (humans included), birds, reptiles, and fish. They
are amoeboid in shape, having clear cytoplasm. Monocytes
have bean-shaped nuclei and constitute 2-10% of all
leucocytes in the human body. Monocytes play multiple roles in immune function.
Such roles include: (1) replenishing resident macrophages under normal
states, and (2) in response to inflammation signals, monocytes
can move quickly (approx. 8–12
hours) to sites of infection in the tissues and divide/differentiate into
macrophages and dendritic cells to elicit an immune response. Half of them are
stored in the spleen”
Wiki.
[2]
“Macrophages are cells
produced
by the
differentiation of monocytes in tissues.
Macrophages
function in both non-specific defense
(innate immunity) as well
as help
initiate specific defense mechanisms (adaptive
immunity) of vertebrate
animals. Macrophages have the unique ability to metabolize one amino acid,
arginine, to either a "killer" molecule (Nitric Oxide) or a
"repair" molecule (Ornithine). Macrophages predominantly expressing
the killer or repair phenotype are now mainly called M1 or M2 macrophages
because these 2 types of macrophages also stimulate T cell responses that
further activate the killer macrophages or T cell phenotype (Th1), or stimulate
antibody production (Th2).[4] Their role is
to phagocytose, or engulf
and then digest, cellular debris and pathogens, either
as stationary or as mobile cells. They
also stimulate lymphocytes and other immune
cells to respond to pathogens.
They are specialized phagocytic cells that attack foreign substances,
infectious microbes, and cancer cells
through destruction and ingestion. They are present in
all living tissues, and have a function
in regeneration. Macrophages are
highly specialized in removal of dying or dead cells and cellular debris.
Macrophages are the predominant cells involved in creating the progressive
plaque lesions of AS”
Wiki. It is
the role of
dealing with oxidative damaged LDL that causes AS.
[3] The
term “lipid” has two meanings: that of
fats including triglycerides, and also any molecules with a fat like appearance
and insoluble in water including heavy esters, alcohols, waxes and closely
related substances such as phospholipids); second meaning fats. Both meanings
refer to compounds with a chain
of single bonded carbons. Though not including cholesterol & sterols by
definition, in this case the KOL means triglycerides and cholesterol, based
upon development of topic. Such usage
has become common.
[4]
The damage to and death of macrophages simply from performing their mop-up
function is self-defeating, in that a greater amount of debris is created than
at the beginning. The pathogen-toxin
evidence supports the view that these reactive chemical attached to LDL and HDL
destroy the macrophages. Evidence
presented in next section.
| Plaque forms in the tunica intima layer |

|
|
|
Pharma’s myth on the cause
of AS: There
are two answer the
standard one spread by pharma and its KOLs,
which promotes drug sales and doesn’t prevent chronic illness. The evidence
that undercuts the cholesterol-LDL
theory has been set out at Cholesterol
Myth, Cholesterol Myth,
History
and FH,
and The great cholesterol
myth
Kendrick
. LDL not only functions to transport
vital cholesterol & fats to cells and organs in need, but also as part of
the immune system. Reading pharma’s account of reactive chemicals attaching to LDL
in the tunica media of the artery walls is not convincing. Simply put, they
observed oxidative damage to
LDL following transport through the endothelial barrier on the artery wall (see
diagram above). But is an area of low
activity, it should be happening at a higher rate in organs of high metabolism
and those like that use in biosynthesis large amounts of cholesterol such as
the goal bladder—but it doesn’t.
Moreover pharma’s KOLs write
of an inflammation response to the damage LDL, but fail to note that pathogens
are also present in the atheroma.
Hundreds of journal article confirm their presence and role in AS.
The KOLs ignore the awkward.[1] They
also ignore the immune system function of HDL and LDL (see links above).
The causes of AS (in order of significance) pathogens: “AS
may be
caused by an infection of the vascular smooth muscle cells. For example, Cytomegalovirus (CMV) infection is also associated
with cardiovascular
diseases.[13] In time, as cells die, this leads to
extracellular calcium deposits between the muscular wall and outer portion of
the atheromatous plaques. The accumulation
of calcium leads to a loss of elasticity and stiffening of the artery as a
whole“ Wiki. This is a gross understatement of their
role: “However,
the cumulative evidence may support that as part of innate immunity,
lipoproteins may also broadly prevent or inhibit bacterial, viral and parasitic
infections. Lipoproteins can detoxify lipopolysaccharide and lipoteichoic acid.
Lipoproteins neutralize a vast of enveloped and non-enveloped DNA and RNA
viruses. Staphylococcus aureus
-toxin is bound and inactivated by purified LDL. LDL also directly binds to some bacteria,” at. Hundreds of journal articles going
back
nearly a century describe the presence of bacteria and viruses in atheroma, and
related affects. “A rapidly-expanding volume of research is implicating common
infectious agents—including the respiratory but Chlamydia
pneumoniae, the ulcer-causing Helicobacter
pylori bacteria, herpes viruses such as
cytomegalovirus, and Herpes simplex
and even dental infections—as playing a direct role in the instigation and
progression of CHD…. A review of thirteen published studies in which
researchers went hunting for the organism [Chlamydia pneumonia] in arterial
tissues showed that the organism could be detected in over half of all
atheromas, but in only 5 percent of adjacent, lesion-free arterial tissue
samples 207-208…. [e]xamined fifty human atheroma specimens, they found that
forty-four percent were positive for one or more strains of periodontal
bacteria,“ p 208, The
Great Cholesterol Con, Anthony Colpo, 2006.
For journal articles go to infection
in artery wall causes CVD and Major Cause
of Atherosclerosis. Infectious agents are the
principle cause of AS, not a minor
cause. It is why over half of all
AMI
occur in those with normal levels of cholesterol and without metabolic
syndrome.
Other factors
accelerate the process started by infectious agents: Thus
the three main causes of AS are oxidation and glycation of LDL
and the presences of virus or bacteria in the artery walls. The role of infection
is a main reason why
over 45% of those with their first MI are in the low risk population. AS causes hypertension by stiffening
the artery walls which increases blood pressure and the risk of thrombosis. The
most significant are reactive chemicals,
which come mainly from external sources such as carbon monoxide, dietary
sugars, other dietary chemical both natural and man-made, and products of
cellular biosynthesis and metabolism.
The main source of carbon monoxide is cigarettes; the sugars come from
carbohydrates. Among the natural
dietary chemicals are trans-
fats and polyunsaturated fats high in omega 6 fatty acids. For detail account
of the role of carbs, of fats in diet and AS.
Hypertension is a
marker for AS. It is the young unstable plaque that leaks and the subsequent
thrombosis (clot) that cause of over 80% of the MIs. Hypertension’s affect
upon progression of AS
and unstable young plaque to MI is minimal; moreover, the drug treatments
pushed by pharma are not worth the side effects. Since blood pressure goes up,
the finding
through imaging of an association with the quantity of plaque, doesn’t prove a
cause, rather hypertension is a result of the AS. This was the wisdom printed
in medical
textbooks in the 1940, and pointed out the futility of drug intervention to
reduce hypertension as to positive endpoint results of death and acute ischemic
events, at. The best choices are the various ways to
reduce the risk for continued development of atheroma, which are detailed at
the end of this paper. What is good for
blood vessels also reduces blood pressure--for more on hypertension and treatments.
“Athero-embolism, cholesterol
embolism, sometimes blue
toe or purple toe syndrome or trash foot or warfarin
blue toe syndrome occurs when cholesterol [and other constituents of plaque] are released
usually from
an atheroma and travels along with the blood stream
(embolism) to other places in the body, where it obstructs blood
vessels. Most commonly this
causes skin symptoms (usually livedo reticularis), gangrene of
the extremities and sometimes renal
failure; problems with other
organs may arise, depending on the site at which the cholesterol crystals enter
the bloodstream. [Other articles list spleen,
pancreas, brain, heart, kidney,
eyes, legs, feet]. When clotting occurs (thrombosis) if in a major coronary
artery it can result in AMI. It
develops about 5% of the time following PCI, may
develop after the commencement of anticoagulants or
thrombolytic medication that decrease blood clotting or
dissolve blood clots thus freeing upon the plaque to travel downstream” Wiki. Cholesterol embolism is very strongly associated
with invasive procedures: confirmed in
20 of 22 patients in a histologically post mortem proven cases. Cholesterol embolism issues became evident
within 3 months, most within 3 weeks, at. This event is typically
attributed to natural events, thus the 5% figure is Wikipedia is quite low[2].
Terming it “cholesterol embolism”
instead of “athero-embolism” is another way that pharma distorts the picture--plaque
is far more than just cholesterol.
[1] If
they didn’t, they would be KOLs.
Ignore
the Awkward is the type of Prof. Uffe Ravnskov book on the cholesterol
myth
[2] “Embolization
of cholesterol crystals from ulcerated atheromatous lesions can produce distinct syndromes that mimic more common
disease processes. Cholesterol emboli can present as renal
failure, hypertension, spells of
numbness, abdominal pain, and myocardial
infarction, or as a multisystem disease that closely
approximates the presentation, clinical course, and even biopsy picture of polymyositis or periarteritis
nodosa.
A review of this problem with particular attention to the clinical presentations
should help in the early diagnosis and treatment of cholesterol emboli and avoid unnecessary and inappropriate
therapies” at The Great Masuerader.
Thrombosis: “(Greek: θρόμβωσις)
is the formation of a blood clot (thrombus; Greek: θρόμβος) inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel is injured, the body uses platelets (thrombocytes) and fibrin to form a blood clot to prevent blood loss. Even when a
blood vessel is not
injured, blood clots may form in the body under certain conditions.
For example, leaking plaque can partially
plug a coronary artery and initiate the clotting process further occluding the
coronary artery and this can result in a heart attack. Hypoxia, oxygen deprivation, occurs and metabolic products
such as lactic
acid can accumulate. A
larger thrombus causing a much greater obstruction to the blood flow may result
in anoxia, the complete deprivation of oxygen and infarction, tissue death.
A clot that breaks free and begins to travel
around the body is known as an embolus.” Wiki.
Myocardial
infarction (MI) or acute
myocardial infarction (AMI)
is the medical term for an event commonly known as a heart attack. It happens when blood stops flowing properly to part of the
heart and the heart muscle is injured due to not getting enough
oxygen. Usually this is
because one of the coronary arteries that supplies blood to the heart develops
a blockage due to
an unstable buildup of cholesterol and fat and foam cells. The event is called "acute" if it
is sudden and serious. The resulting
ischemia (restriction in blood supply) and ensuing oxygen shortage, if left untreated for a sufficient period
of time, can cause damage or death (infarction) of heart muscle tissue (myocardium). A
sizeable proportion of myocardial infarctions (22–64%) are
"silent", that is without chest pain or other symptoms. There are 2
basic types of AMI involving a major
coronary artery: 1) transmural which is associated with AS involving a major coronary artery, and extends through the whole
thickness of the heart muscle. 2)
Subendocordial,
involving a small area in the subendocardial wall of the left ventricle,
ventrical septum, or papillary muscles. For
signs of MI read Heart Attack & Treatment Choices, which also lists risk factors, diagnosis, and treatment
choices, including those supported by marketing science studies and rubber stamped into a protocol by pharma
friendly organizations including the FDA and American Heart Association.
The major reduction in the death rate from MI since the 1980s results from prompt
sublingual 325 mg aspirin and nitroglycerin and the development of thrombolysis
and PCI--not statins as Pharma
teaches. The reduction occurred
prior to
the wide use of statins—though pharma of course claims the credit.
|
“Yet despite these medical advances, with
success in reducing the symptoms of angina and reduced blood
flow,
atheroma rupture events remain the major problem and
still sometimes result in sudden disability and death despite even the most
rapid, massive and skilled medical and surgical intervention available
anywhere today. According to some clinical trials, bypass surgery and
angioplasty procedures have had at
best a minimal effect, if any, on improving overall survival. It is also
clear that both angioplasty and bypass interventions do not prevent future heart attack” Wiki. This
has
been known since the 70s, but by KOLS to physicians, and thus patients.
|
| LDL is the transport system for cells that |
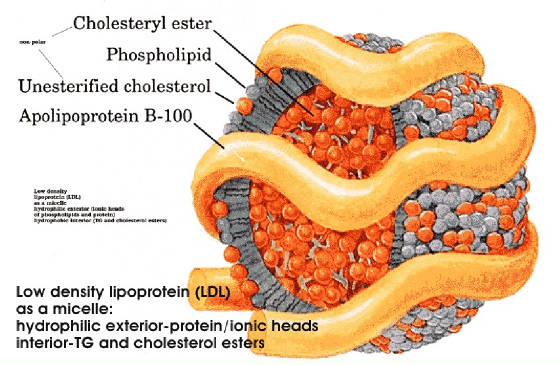
|
| need cholesterol and triglycerides |
Treatments: THROMBOLYSIS “Is the breakdown (lysis) of blood clots[1] by pharmacological means and is
colloquially referred to as clot
busting. It works by stimulating fibrinolysis by plasmin through infusion of analogs of tissue plasminogen activator (tPA), the protein that normally activates plasmin
[body’s method
of breaking down a blood clot.] Thrombolysis
suggests the use of thrombolytic drugs, which
are either derived from Streptococcus species,
or, more recently, using recombinant biotechnology whereby
tPA is manufactured by bacteria,
resulting in a recombinant tissue plasminogen activator or rtPA.
Some commonly used thrombolytics are:
streptokinase, urokinase, and the
recombinant tissue
plasminogen activators (alteplase (rtPA),
reteplase, tenecteplase).
Most
thrombolytic agents work by activating the enzyme plasminogen,
which clears the cross-linked fibrin mesh (the
backbone of a clot). This makes the clot soluble and subject to further proteolysis by other
enzymes, and restores blood flow over occluded blood. Thrombolysis
is used effectively for myocardial infarction, stroke (ischemic
stroke)[4],
massive pulmonary embolism, acute limb ischaemia.
Apart from streptokinase, all thrombolytic drugs are administered
together with heparin[1] (unfractionated
or low molecular weight
heparin), usually for 24–48 hours[2]
while anticoagulants decrease “growth” of a clot, thrombolytic agents actively
reduce the size of the clot” Wiki. The ruptured plaque is now being dissolved and
broken up by the flow of blood, and recapped by endothelial cells. Thrombolysis is commonly used also for
ischemic stroke, massive pulmonary embolism, and acute limb ischemia.
Unfortunately the major benefit for MI and
stroke occurs in the first 90 minutes from symptoms and by 3 hours is not worth
the side effects. Oxygen starved tissue dies quickly. But patients are looking for something to be done;
they get this something.
“PERCUTANEOUS CORONARY INTERVENTION (PCI), commonly known as coronary angioplasty or simply angioplasty, is a non-surgical procedure used to treat
the stenotic (narrowed) coronary arteries of the heart found in coronary heart disease. During PCI, cardiologist feeds a deflated
balloon or other device on a catheter from the inguinal femoral artery or
radial artery up through blood vessels until they reach the site of blockage in
the heart. X-ray imaging is used to guide the catheter threading. At the
blockage, the balloon is inflated to open the artery using water pressures some
75 to 500 times normal blood pressure (6 to 20 atmospheres). Usually, patients receive medication that will
relax them to protect the arteries against spasms. [The best drugs are
morphine and lidocaine. Pharma prefers
tranquilizers
for they cloud cognitive function and thus promote over treatment.]
Patients are typically able to walk within
two to six hours following the procedure and return to their normal routine by
the following week.[2] A stent is often placed at the site of blockage
to
permanently open the artery. Other
procedures are rotational or laser atherectomy and brachy-therapy (use
of radioactive source to inhibit restenosis)” Wiki--a link there
is to BBC film showing
PCI. Unfortunately
like thrombolysis, the major benefits occurs in the first 90 minutes from
symptoms of MI or stroke, and by 3 hours is not worth the side effects. Oxygen
starved tissue dies quickly.
COMPARISON OF PCI TO THROMBOLYSIS.
Thrombolysis has a 10% mortality, compared to a 7% PCI (average wait times 112 minutes) in trial of 4003
patients.[3] These trial results
are applicable to only
about 15% of all acute events because of the rapid response time (another
example of pharma clinical trials flawed by designed so a s to promote
marketing objectives). PCI when
available within an hour in the clinic is superior to thrombolysis (only a
small percentage of patients meet these criteria). Patients who experience swelling, bleeding or pain at the
insertion site, develop fever, feel faint or weak, notice a change in temperature or color
in the arm or leg that was used or have shortness of breath or chest pain should immediately seek
medical help. The risks from both
procedures are greatly
under-reported. Deaths are routinely
attributed
to the natural course of the AMI
and
a subsequent stroke or cholesterol embolism attributed to existing AS,
and not to the procedure. Guidelines call for intervention within 6
hours, results support significant benefit within 1.5 hours of first
symptom. After that side effects
entail
a negative result.
Elective Treatments (usually performed months after an MI):
The coronary vessel with hard stable plaque is not the site of the MI[4]. Unstable
plaque causes 90% of the MIs; thus
PCI and bypass surgery are ineffective at reducing mortality or a second MI. Studies
have failed to find reduction in hard endpoints for angioplasty vs. medical
therapy for stable angina patients. PCI
and bypass surgery are about 60% effective after 5 years at significantly
mitigating angina pain. Wiki. However, similar results
occur for angina without the procedure after 5 years due to revascularization. Elective bypass surgery causes pump
head (significant
cognitive decline) in 25 plus percent of patients, and there are other side-effect. “It is also clear that both angioplasty and bypass
interventions do not
prevent future heart
attack”
Wiki.
Polypharmacy:
the use of 5 or more drugs following an MI “a legitimate treatment regime
could include a statin, an ACE inhibitor & a beta-blocker [for
hypertension], [low dose] aspirin, paracetamol [Tylenol], anticoagulant, and an
antidepressant’
Wiki, and an
arrhythmia drug. Costs often run
over
$60,000 yearly. Pharma knows that
those
who undergo radical interventions--bypass, angioplasty, and thrombolysis--are
more likely to comply with the drug cocktail.
The effects of these drugs
on
quality of life is significant; most common is major cognitive decline and
myopathy.
Angina: “AGINA PECTORIS – commonly known as angina – is chest pain due to ischemia of the heart muscle, generally due to obstruction or spasm of
the coronary arteries.[1] The main cause of Angina pectoris is
coronary artery disease, due to AS of the arteries feeding the heart.
The term derives from the Latin angina ("infection of the throat") from the Greek ἀγχόνη ankhonē (strangling),
and the Latin pectus (chest), and can therefore
be
translated as "a strangling feeling in the chest". There is a weak relationship between severity
of pain and degree of oxygen deprivation in
the heart muscle (i.e.,
there can be severe pain with little or no risk of a Myocardial infarction and a heart attack can occur without
pain). A study of 303 cases of
angina found that 1 in 4 men having a heart attack within 5 years and one in 8
for women. About 30% of those over
the
age of 55 will die within 8 years. Half
of those sustaining an MI have angina following it. Only 23
percent of infarctions were preceded by angina.
STABLE ANGINA: Also
known as effort angina,
this refers to the more common understanding of angina related to myocardial
ischemia. Typical presentations of stable angina is that of chest discomfort
and associated symptoms precipitated by some activity (running, walking, etc.)
with minimal or non-existent symptoms at rest or with administration of
sublingual nitroglycerin. Symptoms
typically abate several minutes following cessation of precipitating activities
and reoccur when activity resumes. In this way, stable angina may be thought of
as being similar to intermittent
claudication symptoms.
UNSTABLE ANGINA: “Unstable angina (UA) (also "crescendo angina;" this is a form of acute
coronary syndrome) is
defined as angina pectoris that changes or worsens. It has at least one of these three features: (1) occurs at rest (or with minimal
exertion), usually lasting >10 min; (2) severe and of new onset (i.e.,
within the prior 4–6 weeks); (3) ours with a crescendo pattern (i.e.,
distinctly more severe, prolonged, or frequent than before).Studies show that
64% of all unstable anginas occur between 10 PM and 8 AM when patients are at
rest. This cap (atherosclerotic plaque) may rupture
in unstable angina, allowing blood clots to precipitate and further decrease
the lumen of the coronary vessel. This explains
why an unstable angina
appears to be independent of activity--most often between 10 PM and 8 AM.” Wiki. Too much is made of unstable angina as a way
to sell drugs and bypass and PCI. AVOID:
Beta blockers and calcium channel blockers act to decrease the heart's workload,
and thus its
requirement for oxygen, but the effect is minimal and the side effects
long-term are serous, and they increase mortality. A heart whose function has been compromised
by long-term drugs that effect nerves to reduce blood pressure is more likely
to fail under stress of an AMI. Only
looking through a selective window are they justified by clinical trials.
Nitroglycerin is best for angina pain and
best long term is treatment designed to “stopping
and even partially reversing the
atheroma growth process” Wiki. Angina gradually
diminishes over several years through the process of revascularization.
Imaging: it has limitations for
a number of reasons. First, over
half of
all AMI occur without significant clinical signs; viz. they don’t show up on imaging. Second, over 90% of events are not caused by
occluded coronary vessels, but by young unstable plaque with occlusion under
50%. These vessels don’t show
up under
with imaging as diseased. Third,
there
are no effective treatments for those vessels with unstable plaque, even if
they were revealed. Fourth, for
the
occluded vessels interventions such as PCI and bypass are ineffective, thus the
knowledge doesn’t affect the course of events. Fifth, angiogram has significant risk of both
major and minor events, one study found an increase of 23%. If you must know, the best indicator is a
sonogram of the carotid artery; and hypertension is also an indicator.
Conclusion:
Imaging gives to diagnosis the sound of authority; thus technology is a sales tool for additional
treatments.
|
Two essential points for understanding
why the recommendations below are contra pharma’s position. One that
pharma has tobacco ethics: the rule by which corporations function to
maximize profits. Second, applying
this rule, they do all that is necessary to promote their patented drugs, and to reduce the usage of off-patent
drugs. Research is done for marketing goals,
thus bias is the norm. The drugs listed below have a compelling
body of evidence published at /rc
, diet at /rh. How pharma applies tobacco ethics and
thus influence the practice of medicines is at bad pharma, /rep, and Junk treatments, There are links to a collection of the best
of university lectures and documentaries on the issues raised.
|
[1] A safer course
would be that of taking a
larger dose of aspirin, 975 mg. Contrary
to Big PhARMA, it is a wonder drug, at aspirin.
[2]
Absolute
Contraindications: Previous
intracranial bleeding at any time, stroke in less than 6
months, closed head or facial trauma within 3 months, suspected aortic
dissection, ischemic stroke within 3 months (except in ischemic stroke within 3
hours time), active bleeding diathesis, uncontrolled high blood pressure
(>180 systolic or >100 diastolic), known structural cerebral vascular
lesion, arterio-venous malformations, thrombocytopenia, known coagulation
disorders, aneurysm , brain tumors,
pericardial effusion. Relative contraindications: Current anticoagulant use, invasive or
surgical procedure in the last 2 weeks, prolonged cardiopulmonary resuscitation
(CPR) defined as more than 10 minutes, known bleeding diathesis, pregnancy,
hemorrhagic or diabetic retinopathies, active peptic ulcer, controlled severe
hypertension.
[3] Another
trial 3750 patients had results favoring PCI 12% mortality versus 15% for thrombolysis; and the incidents or
stroke and subsequent MI similarly
favored PCI. A 3rd comparative
article, a meta-analysis had short-term deaths 7% vs. 9% for thrombolysis,
and combined end points of 8 vs. 14%.
PCI is modestly better than
thrombolysis.
[4] “Atherosclerotic lesions and atherosclerotic plaques are separated into
two broad categories: Stable and unstable (also called vulnerable). The pathobiology of atherosclerotic
lesions is very complicated but generally, stable atherosclerotic plaques,
which tend to be asymptomatic, are rich in extracellular
matrix and smooth
muscle cells, while, unstable plaques
are rich in macrophages and foam cells and the
extracellular matrix separating the lesion from the arterial lumen (also known
as the fibrous cap) is usually weak and prone
to rupture. Upon formation, intraluminal
thrombi can occlude arteries outright (e.g. coronary occlusion), but more often
they detach, move into the circulation and eventually occluding smaller
downstream branches causing thromboembolism (for example, a stroke is often caused
by thrombus formation in the carotid arteries)” Wikipedia.
HEALTHFUL CHOICES
Lifestyle
makes a difference:
The greatest gains are from weight
control, low-carbohydrate-sugar diet to prevent insulin resistance, cessation
of smoking, and vigorous
exercise.
Rapping the heart in a layer of fat and making the heart pump harder
through miles of blood vessels are consequences of obesity. Moreover with obesity, adipose tissue affects
the feedback mechanism that regulates insulin; thus the risk of type-2 diabetes
increases by 30 fold. Diabetes causes
a
higher level of blood borne sugars thus increases glycation which causes
endothelia dysfunction. Diabetes
causes
red blood cells to leak out of capillaries which cause an immune response by
macrophages. For these reasons diabetes
doubles the rate of MI. Diabetes shortens life an average of 5 years
and with obesity more. The carbon
monoxide--a reactive chemical that damages LDL-- from tobacco doubles the rate MI.
A pack-a-day smoker shortens their life on an average 12 years. Carbon monoxide promotes the production of
unstable plaque, thus with cessation,
the
risk for MI dramatically drops over
the next 5 years. Vigorous
exercise
strengthens the heart, better vascularization, lowers blood sugar level, &
has anti-inflammatory effect thus and healthful
effects
upon the epithelium (cell walls) of arties. Controlling for lifestyle contravening
variables, senior runners extended life 8.7 years, & it improves quality of
life. “Exercise capacity
is a best
predictor of mortality” NEJM.
Diet makes a difference, but not the diet that
pharma & our government teaches which promote the fat-cholesterol
myth. In 11 out of 12 studies reviewed in Wikipedia,
results showed no benefit from low fat, or increased ratio of polyunsaturated
fats “A meta-analysis of 21 studies considered the effects of
saturated fat intake and found that Intake of saturated fat was not associated
with an increased risk of coronary heart disease [CHD], stroke, or cardiovascular disease [CVD]" Wiki. The initial cause of CVD process is pathogens, the process is accelerated
by glycation throughout the body and insulin resistance, both of which are
promoted by a high refined carb diet and especially sucrose which is one half
fructose. A high sugar diet
(especially fructose) is associated with insulin resistance (high blood sugar
level), diabetes, and metabolic syndrome; all are causal factors for AS.
As stated before, most fats are not the culprit: “Indeed,
recent prospective cohort studies have not supported any significant
association between saturated fat intake and cardiovascular risk” BMJ. Instead,
saturated fat has been found to be protective. Trans-fats and
high amount of omega-6 fatty acids[1]
(main source is vegetable oil); both promote CVD. In most countries trans-fats are effectively
banned (not the US), and the ratio of the omega 6 acids can be reduced by decreasing
the use of vegetable oils with the exception of coconut, palm kernel, and olive
oils. Go to for diet and for in depth supporting
evidence on carbs, and fats.
Aspirin: “Irreversibly blocks
the formation of thromboxane A2 in platelets, producing an inhibitory effect on platelet aggregation. This antithrombotic property makes
aspirin useful for reducing the incidence of heart attacks. Since platelets have no DNA, they are unable
to synthesize new PTGS once aspirin has irreversibly inhibited the enzyme, an
important difference with reversible inhibitors…. aspirin induces the formation
of NO-radicals in the body, which has been shown in mice to have an independent
mechanism of reducing inflammation.” Wiki. The platelet
effect reduces thrombosis risk over 40% (with 325 mg) and the NO (nitrous
oxide) in slowing/preventing atheriogenesis. Atherogenesis
slowed: “strong evidence that AS is slowed down in a dose term …
aspirin,” and
stopped. This effect is
dose dependent, comparing
900 to 50 mg of aspirin. At 325 mg with
meals aspirin has an anti-inflammatory
effect and thus prevents
the formation of young unstable plaque, the cause
of ischemic events. Benefits; Various
mechanisms: By NO endothelial cells
from
oxidative
damage, inhibits leukocyte
attacks, cytokinies, & CD36. The anti-inflammatory effect has other healthful
consequences. Also prevents cancer
and cures it by
stimulating the body’s necrosis factor.
And has other
benefits. The risk of bleeding is
greatly exaggerated by pharma
who opposes prevention of chronic conditions through their numerous marketing
clinical trials and use of opinion leaders to instruct physicians in their
required continuing education classes (the same has been done with estrogen). The increased risk of major bleed with
aspirin long-term is 4%. Aspirin is both
effective at preventing cancer and reducing the risk of it become fatal
(metastatic).
Estradiol
with progesterone (natural HRT, NHRT): Estrogen is why women prior to menopause don’t
have cardiovascular disease. Estrogen
lowered by 20% cholesterol, 37% LDL (bad cholesterol) and raised by 14% HDL 14%, extends life 2.1 years, Braunwald,
Heart Disease …, 5th Ed, 1997, p 1708 tables. “Estrogen-replacement therapy decreases
CAD morbidity and CAD mortality … was 0.56
compared to subjects not taking estrogen” [a 44% reduction] Braunwald supra
1142. Another study found a 50% reduction in CHD.
Estradiol blocks
oxidation of LDL to prevent AS.
“Estradiol
completely reverses the effects induced by
OX-LDL on the DDAH/ADMA/NO pathway,” Avoid MPA and LNG (levonorgestrel). Another study found 26 deaths for estradiol vs. 56 for
placebo. A meta-study found
a 50% reduction of Coronary Heart Disease.
AHA study explains
mechanisms of cardio protection. Angina pain (cardiac syndrome X) associated with low estrogen, treated. Estradiol
plus progesterone for CVD & death is the best HRT. Other benefits of natural HRT: the
prevention of osteoporosis, Alzheimer’s
disease, colon cancer, and arthritis.
Testosterone: Prevents metabolic syndrome MetS (poor cholesterol profile,
obesity, and
high blood pressure): “Emerging evidence
suggests that testosterone [TTT]
therapy
may be able to reverse some aspects of metabolic syndrome” And another. “These
results suggest that low SHBG [sex hormone-binding globulin] and/or AD
[androgen deficiency, TTT] may
provide early warning signs for cardiovascular risk and an opportunity for early intervention
in non-obese men.” In a matched study followed ten years
published by the AHA found that the
lowest quarter of men were 41% more likely to die from cancer and
cardiovascular disease compared to the highest quarter. Low TTT is
associated with cardiovascular disease. TTT
Inhibits atherogenesis: in a survey paper,
“Positive correlation between total or free testosterone level and HDL
and a negative association the LDL” and. Conclusion: “A
normal physiological level of TTT in men protects against the development of
high cholesterol, insulin resistance, hypertensions,
clots that cause heart attacks,
obesity, and increased waist:hip ratio, all of which predispose to the
development of CVD. Low or low normal
TTT is implicated in the pathogenesis of acute MI and acute stroke.
The decline of TTT with age may explain the
greater risk of CVD with advancing
years” [medical terminology simplified by jk].
TTT is good for your heart, muscles, and blood vessels. Heart Attack, after controlling for
factors low TTT associated with MI, positive effect upon fibrinolytic pathway, reduces angina. Among
other benefits of TTT are improved libido, quality of life, & mood
elevation. It has positive effects
upon
cardiovascular system because of reduced fat and insulin resistance, reduces
inflammation, promotes physical activity, and increases muscle strength—the heart
is a muscle.
Coenzyme Q10 (CoQ10, Q10):
For heart
failure (HF): the heart isn't
able to adequately pump blood, thus it pools in parts of the body, such as the
lungs and legs. “Several clinical studies suggests that Q10 supplements
help reduce
swelling in the legs; reduce fluid in the lungs to making breathing easier; and
increase exercise capacity in people with heart failure, and reduces hospital admissions by 61%”, similar, also, long-term and safety. After Heart Attack and Angina
pain: A clinical
study found that people who took daily CoQ10 supplements within 3 days of a
heart attack were less likely to have subsequent heart attacks, less chest
pains, die of heart disease. The capacity for exercise improved
about 30% for those with chronic heart failure on taking Q10, also. High blood pressure: In a meta-analysis of 12 clinical studies, Cochrane concluded that Q10 lowers systolic blood pressure
by up to 17 mm Hg and diastolic blood pressure by 10 mm Hg, probably from improved heart functions—that is greater than any hypertensive drug. Bad
cholesterol: Q10 attaches to LDL. It reduces oxidative damage
and thus slows atherogenesis. The mitochondria produce ATP, the energy
source for nearly all bodily functions. Q10
protects the mitochondria from oxidative damage, and thus will very
significantly improve, when taken long term endurance for those over 60 years
and through fitness improves cardiovascular functions, reduces insulin
resistance, and like. The decline in
function of the mitochondria is the reason for the dramatic drop in endurance
of the elderly. The increased production
of ATP entails that the elderly are more likely to survive an MI. The anti-oxidant
effect in the mitochondria
and upon atherogenesis requires Q10 taken life-long. There are numerous other
benefits including
improving blood sugar level in diabetics, for prevention of Parkinson’s
disease, migraines, and macular degeneration, and it should be used with statin
therapy, since stains partially block Q10 production. It is natural with no
known side effects even
at a high dose of 2,400 mg daily.
|
There is a large body of clinical
trials and epidemiological studies that have shown that cholesterol and high saturated
fat diet have no effect upon promotion of CVD, and conversely that a low-fat,
low-cholesterol diet is not cardiovascular protective (see Cholesterol
Myth). As stated prior pathogens within the tunica
media of the artery and the immune response is the primary cause, thus drugs
listed below to lower cholesterol are ineffective though they are much safer
than Statins. Since so many believe
in the cholesterol
myth, the natural method of lowering blood cholesterol with niacin and its
inositol form are included below. Also
included is exposure of hypertension myth as a cause for adverse events—it is
merely a symptom of AS and thus a sign of CVD, not a cause.
|
[1] High
ratio of omega 6 to omega 3, omega 6 occupies the pathway in which omega-3 is
converted to an inflammation modulator.
Ancestral diet was low in vegetable oil had a ratio between 1:1 to 6:1of
omega-6 to omega-3; western diet the ratio is 16:1. Consumption of trans fats is associated with
inflammation biomarkers and endothelial dysfunction, at.
Niacin improves cholesterol profile by
lowering of plasma triglycerides mobilization from adipose tissue, and
inhibiting hepatocyte diacylglycerol acyltransferace synthesis of triglyceride
thereby lowering cholesterol and thus “inhibits the synthesis of
apo-lipoproteins and the influx of free
fatty acids (FFA) into the
liver, which is the precursor of triglycerides.” “A single dose
of niacin 200 mg given in the
fasting state [at bedtime] provides a
prompt and marked fall in serum FFA
level, with a rebound after some hours. A
comparable fall in plasma FFA occurs
normally following a carbohydrate-containing meal, when adipose tissue
lipolysis [making lipoproteins] is
inhibited by insulin, and re-esterification of FA in adipose tissue cells is
increased by glucose. Therefore,
the FFA level is usually low during
the day, when carbohydrates are the predominant source of calories [thus
preventing niacin and statins from reducing FFA]. Lipolysis
becomes active in the post-absorptive state at night,
when the FFA-level is approximately
double the daily mean level. “Oral
administration
of niacin … during the day does not
appreciably alter this pattern.” This is
why blood work requires fasting, and why niacin and IHN should be taken at night,
when the insulin level is low. Thus a low
dose extended release at night-- 200 to 500 mg--is sufficient. Regular
niacin has a peak in 30 minutes and a half-life under 1 hour. Pharma’s recommendation of a mega dose
of niacin (ignores INH) creates very low compliance due flushing, and during
the day for minimal effectiveness. This
pattern of marketing first is the norm for Pharma. Since FFA are modified and
packaged with cholesterol in LDL, niacin lowers the level of LDL.
Inositol
hexanicotinate (IHN, a source of niacin): The literature is thin,
since Pharma members won’t research a flush-free, effective treatment for high
cholesterol. Though IHN releases niacin, it does at too low a rate to affect the same bio-pathway as niacin (peak for
Niacin is 45 minutes, IHN 8 hours). (A
criticism by Pharma of INH, but shown false in a quality study using blood
samples drawn at night). INH
affects Free Fatty Acids (FFA) like niacin.
“FFA is a precursor of plasma triglycerides.
Lipolysis becomes active in the
post-absorptive state at night,
when the FFA-level is approximately double the daily
mean level…. The
Xanintol esters and IHN were superior at lowering
FFA,” at Eur. J.
Clin. Pharmacol. 16, 11-15 1979. In
another study, “At 6 weeks of usage [1650 mg IHN] found a nearly
20% improvement in
cholesterol profile”.
The evidence supporting the use of extended
release niacin and inositol are about equal, thus no preference is expressed
here.
Hypertension: Hypertension is a result of AS,
thus lowering blood pressure has little effect upon ischemic
events. Treating blood pressure
is like
treating fever; it is treating an effect of rather than a cause.
Treating the effect has little benefit, but
for pharma. Instead treat the causes
of
atherogenesis which produces young unstable plaque. Start with lifestyle
changes of exercise,
weight control, exercise, and healthful diet low in salt & refined
carbohydrates. Take Q10, aspirin,
and hormone
replace if suitable. This approach
will lower
blood pressure while reducing risk of adverse events. Short
of malignant hypertension (systolic under 180 and diastolic under 110) don’t
attempt to lower blood pressure with drugs.[1] Moreover blood pressure fluctuates during the
day and is significant, and dependent upon situation when taken. Relax when blood pressure is taken; it will
reduce systolic pressure by at least 10.
“One study found that 41%
of
patients 50 and older who were carefully taken off their high blood pressure
medications did not need them, having normal blood pressure 11 months after the
drug was stopped”18
Worst Pill. “Only
the thiazide and loop diuretics have good evidence of beneficial effects
on important endpoints of hypertension, and hence, should usually be the first
choice when selecting a diuretic to treat hypertension. They are the recommended as first-line
treatment in the US (JNC VII) [5] and European (ESC/ESH) [6] guidelines…. Thiazide diuretics also increase calcium
re-absorption at the distal tubule” Wiki.
Thiazides are “associated with an increase in bone mineral density and
reduction in fracture rates attributed to osteoporosis” Wiki. And their
cost is
under $100/year. The other drugs
for
hypertension are not worth their side effects.
|